The panel discussion summarized:
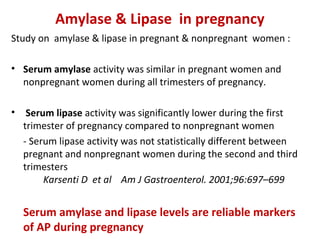
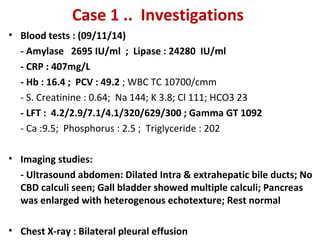
1) Serum amylase and lipase levels are reliable markers for acute pancreatitis during pregnancy.
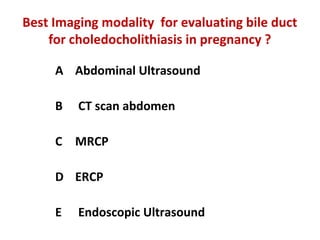
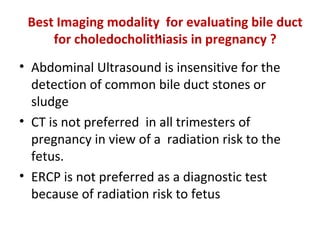
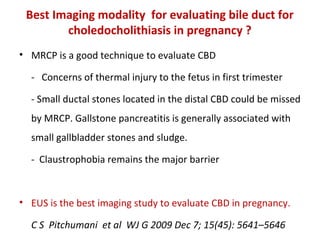
2) MRCP is the best imaging modality for evaluating the bile duct for choledocholithiasis in pregnancy due to lack of radiation exposure, though EUS provides the highest accuracy.
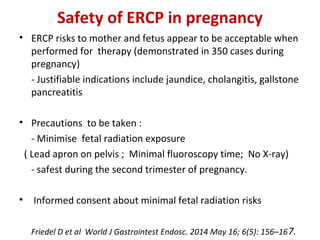
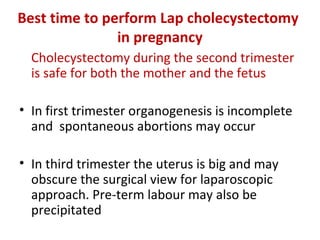
3) Therapeutic ERCP can be performed safely in pregnancy with precautions to minimize radiation exposure to the fetus, and is safest during the second trimester.