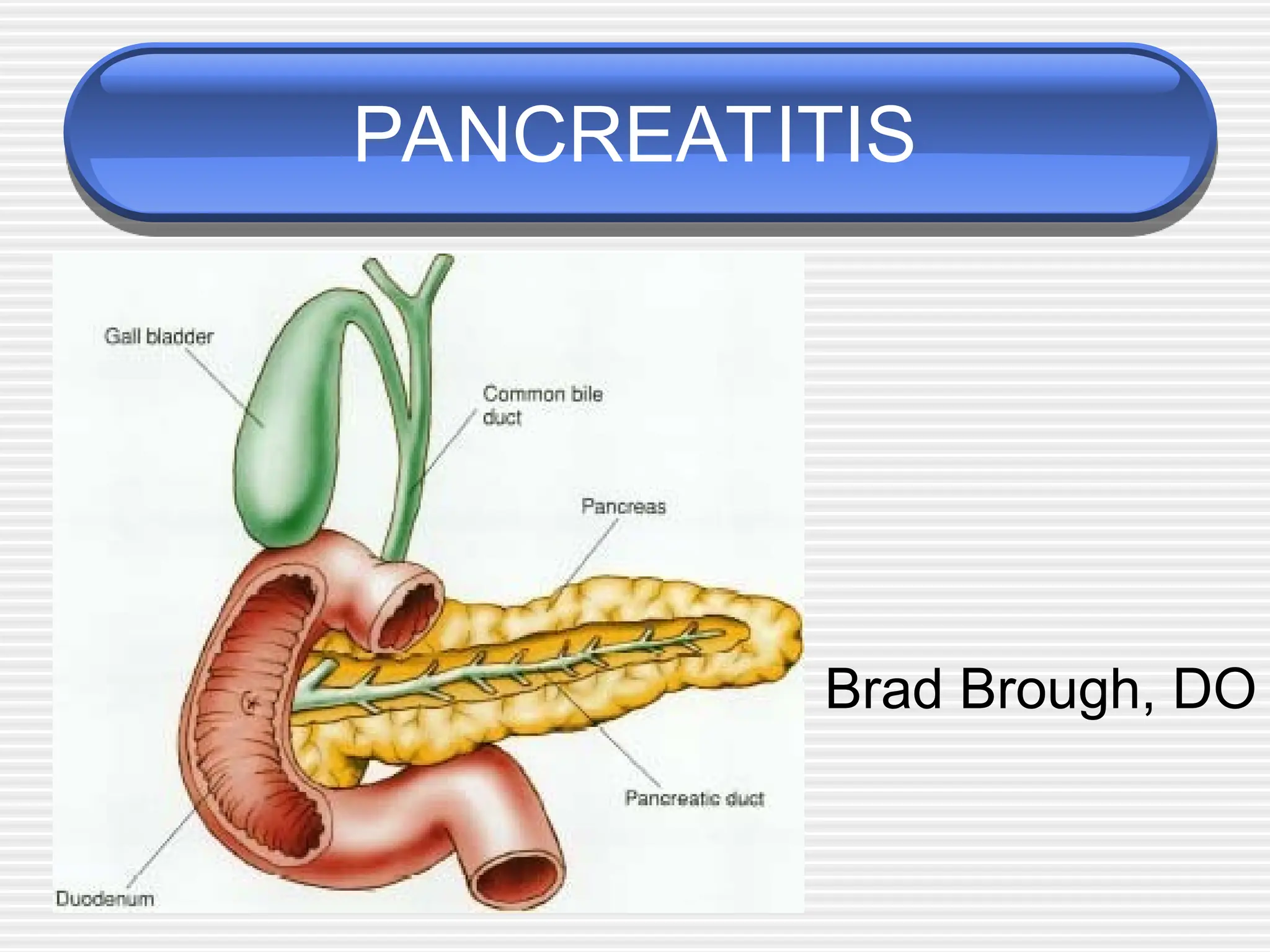
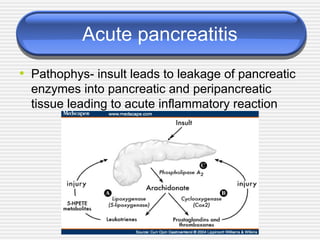
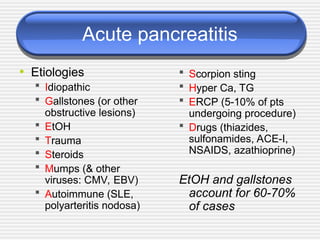
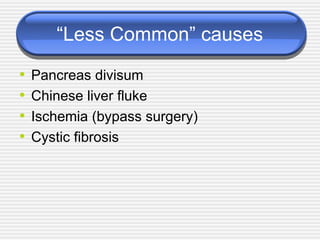
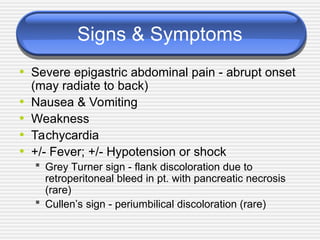
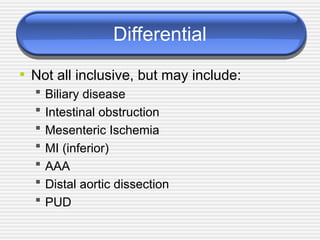
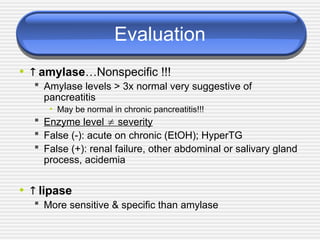
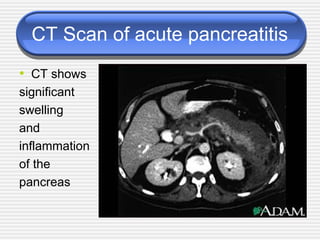
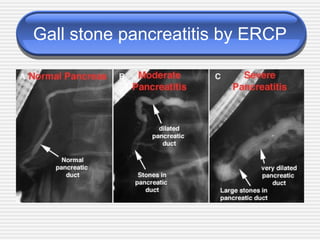
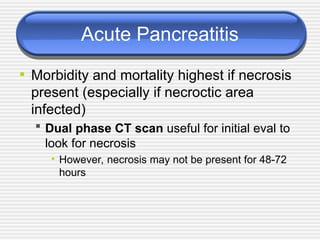
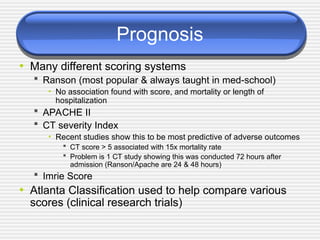
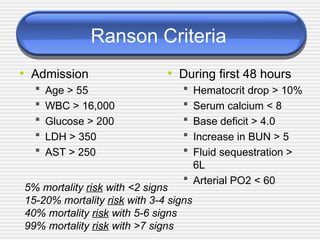
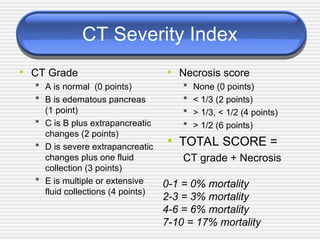
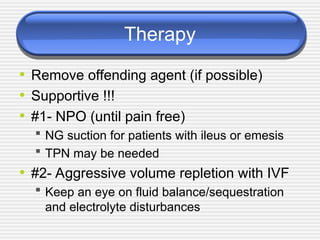
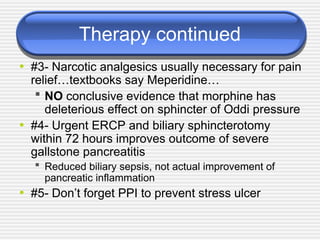
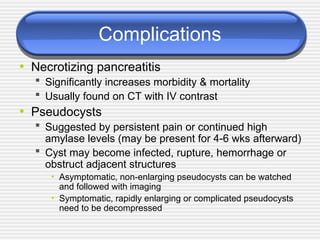
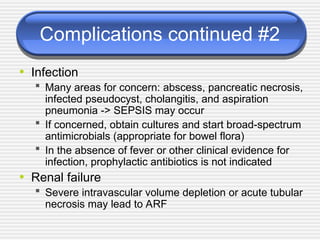
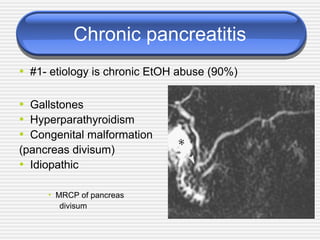
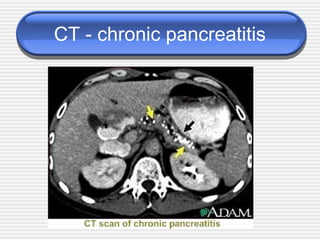
The document provides a comprehensive overview of pancreatitis, focusing on its pathophysiology, causes, symptoms, evaluations, treatments, and complications. Key etiologies include gallstones and alcohol, with critical signs such as severe abdominal pain and diagnostic evaluations highlighting elevated amylase and lipase levels. Management involves supportive care and addressing the underlying cause, with more severe cases potentially requiring ICU admission and having a high mortality rate.