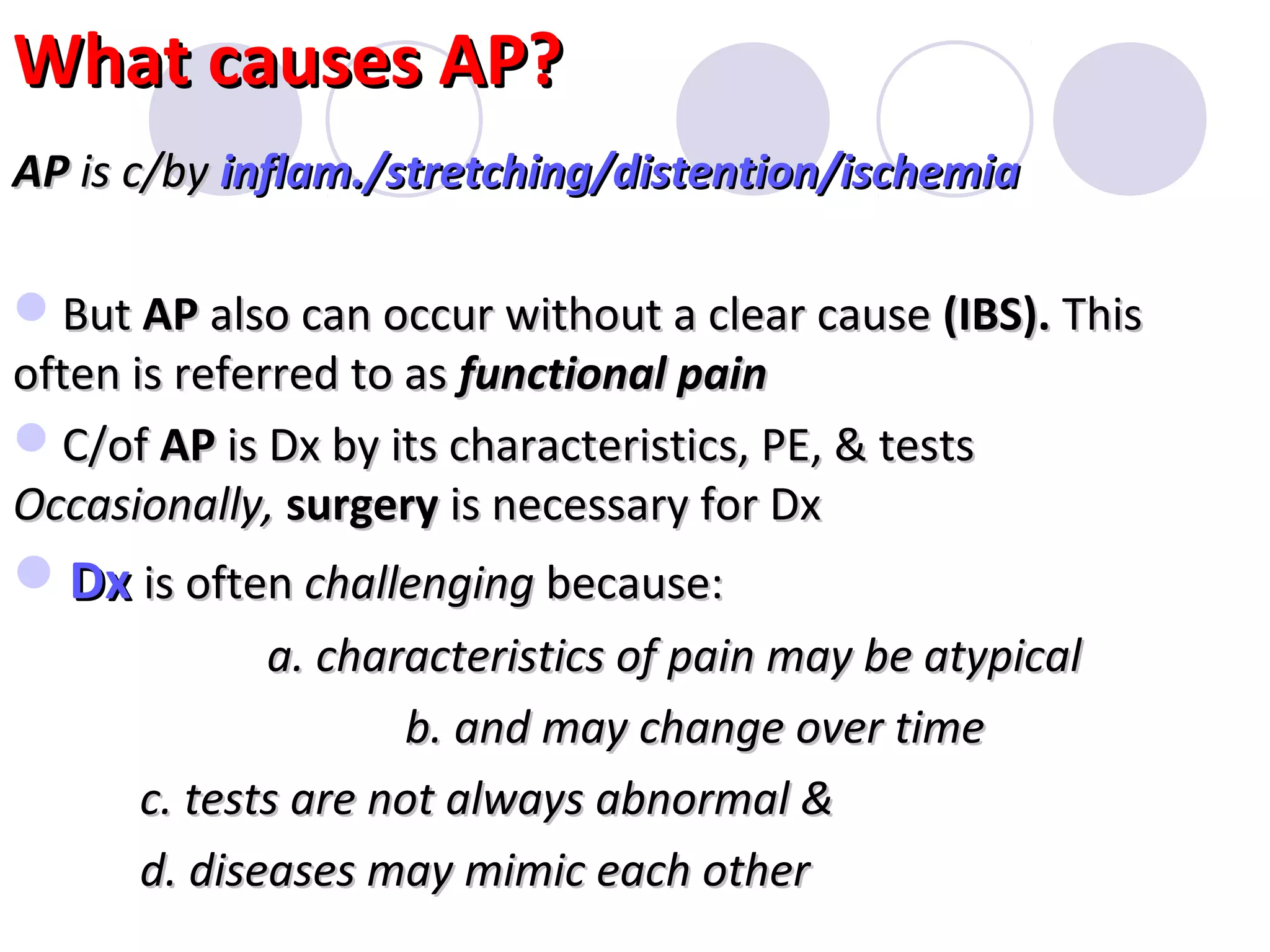
The document discusses abdominal pain, its causes, characteristics, and approaches to diagnosis. It notes that abdominal pain can arise from abdominal wall or organs and may be difficult to localize. Common causes in children include constipation, gastroenteritis, and appendicitis, though some cases require urgent evaluation. Diagnosis involves considering characteristics of the pain, physical exam, and test results. Referred pain is also discussed.