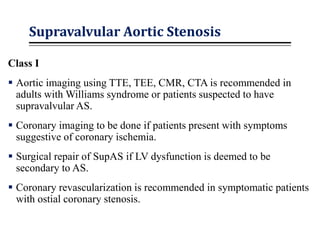
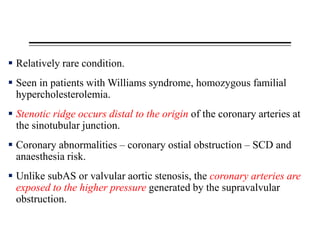
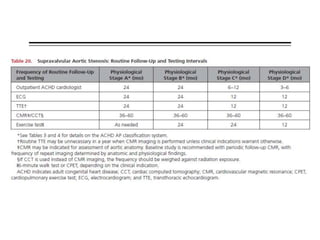
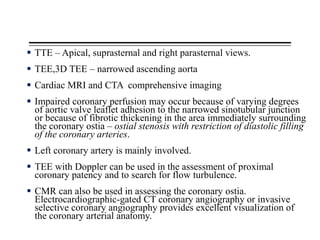
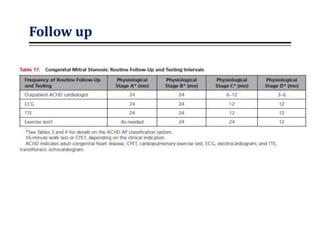
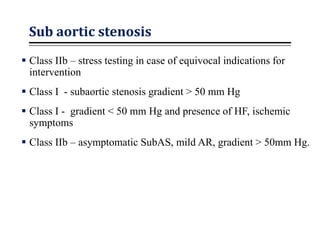
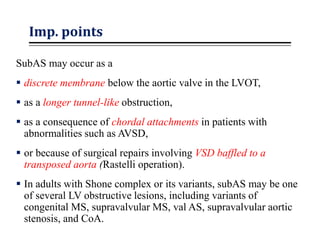
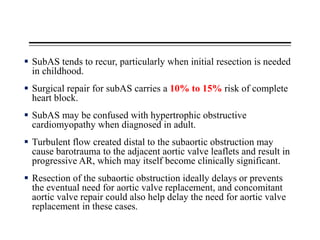
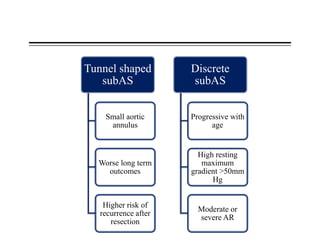
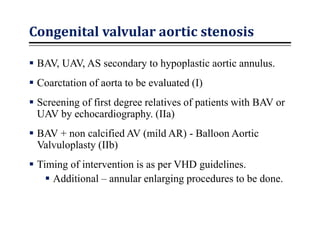
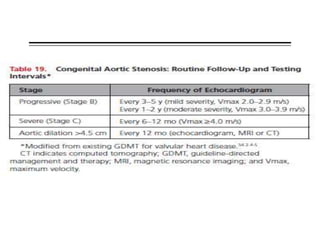
This document summarizes guidelines for treating various left-sided obstructive cardiac lesions. It discusses evaluation and treatment recommendations for conditions like cor triatriatum, congenital mitral stenosis, subaortic stenosis, congenital valvular aortic stenosis, coarctation of the aorta, Turner syndrome, aortopathies, bicuspid aortic valve with aortopathy, supravalvular aortic stenosis, and provides details on diagnostic imaging and surgical repair. The guidelines emphasize evaluating for associated abnormalities, identifying risk factors for complications, and intervening based on symptom status and hemodynamic severity.
![ Although patients with conotruncal abnormalities (TOF,
dextrotransposition of the great arteries [d-TGA] after arterial
switch, pulmonary atresia with VSD, truncus arteriosus) commonly
have aortic diameters of 40 mm to 50 mm, aortic complications are
extremely rare (only 6 published case reports).
Risk factor management such as control of hypertension is
important.
There are no RCTs evaluating the efficacy of medical therapy to
reduce the rate of progression of aortic dilation or incidence of
aortic dissection in this population.](https://image.slidesharecdn.com/achdpartii-200508151030/85/ACHD-Guidelines-part-II-21-320.jpg)