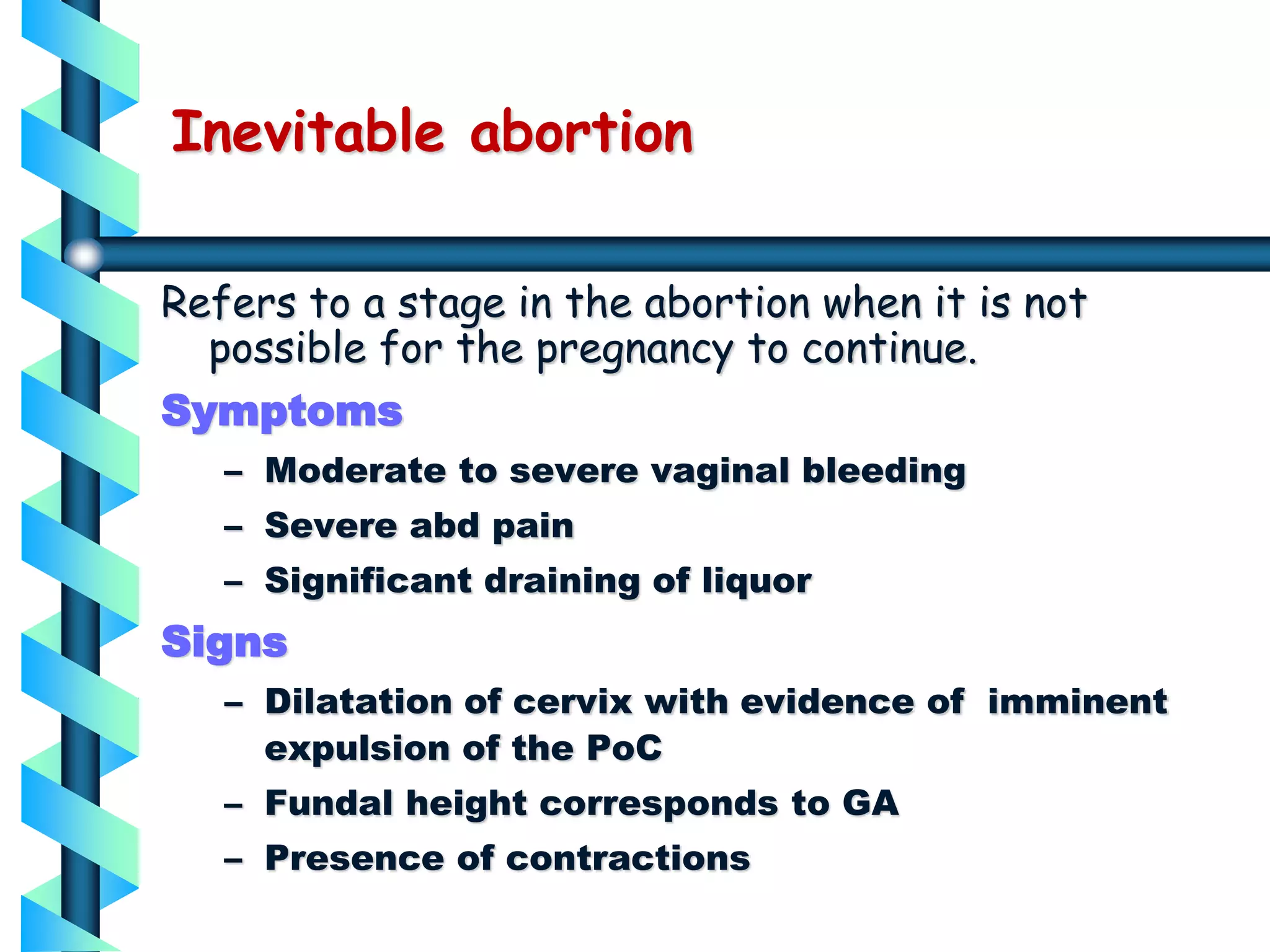
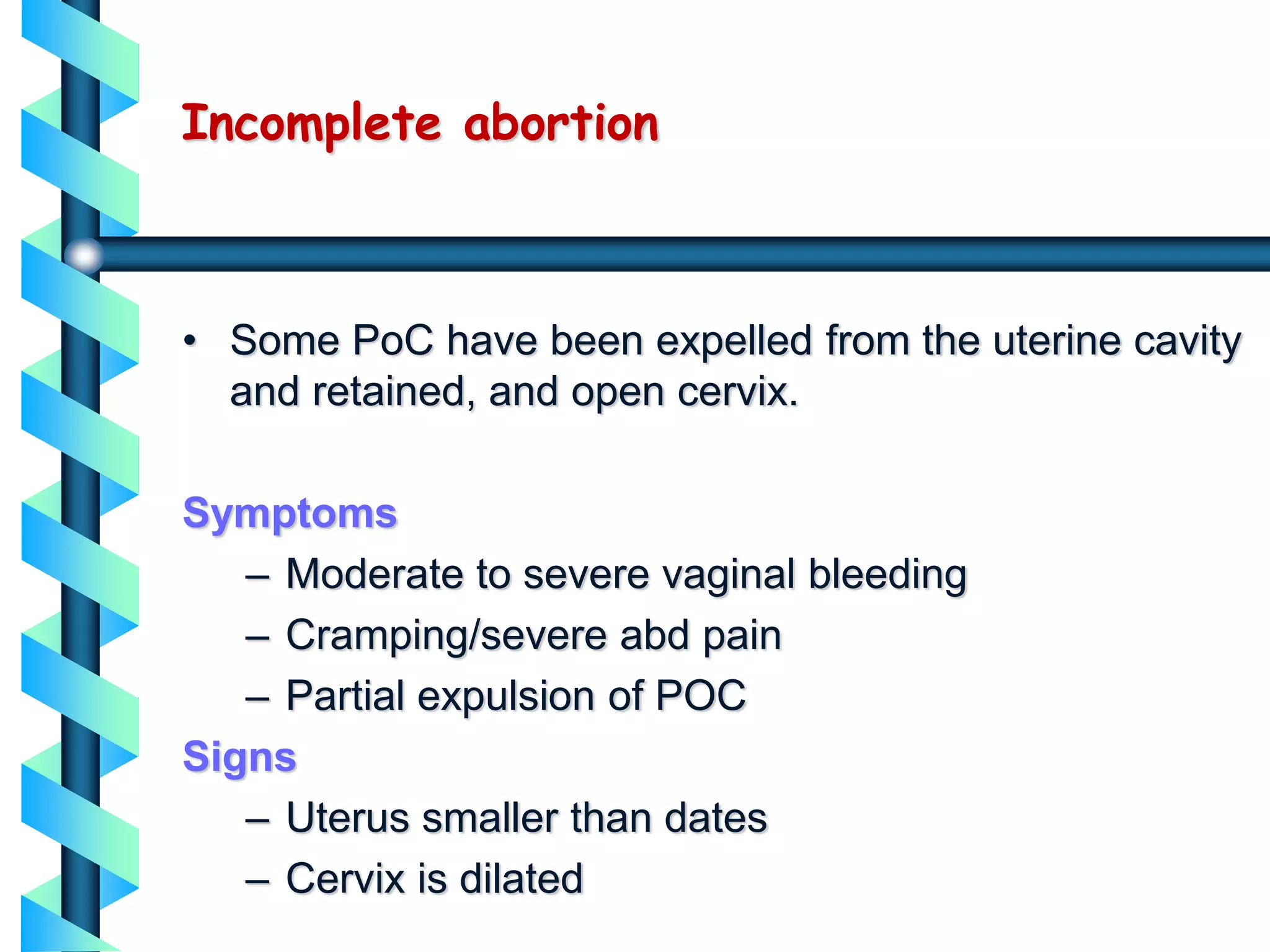
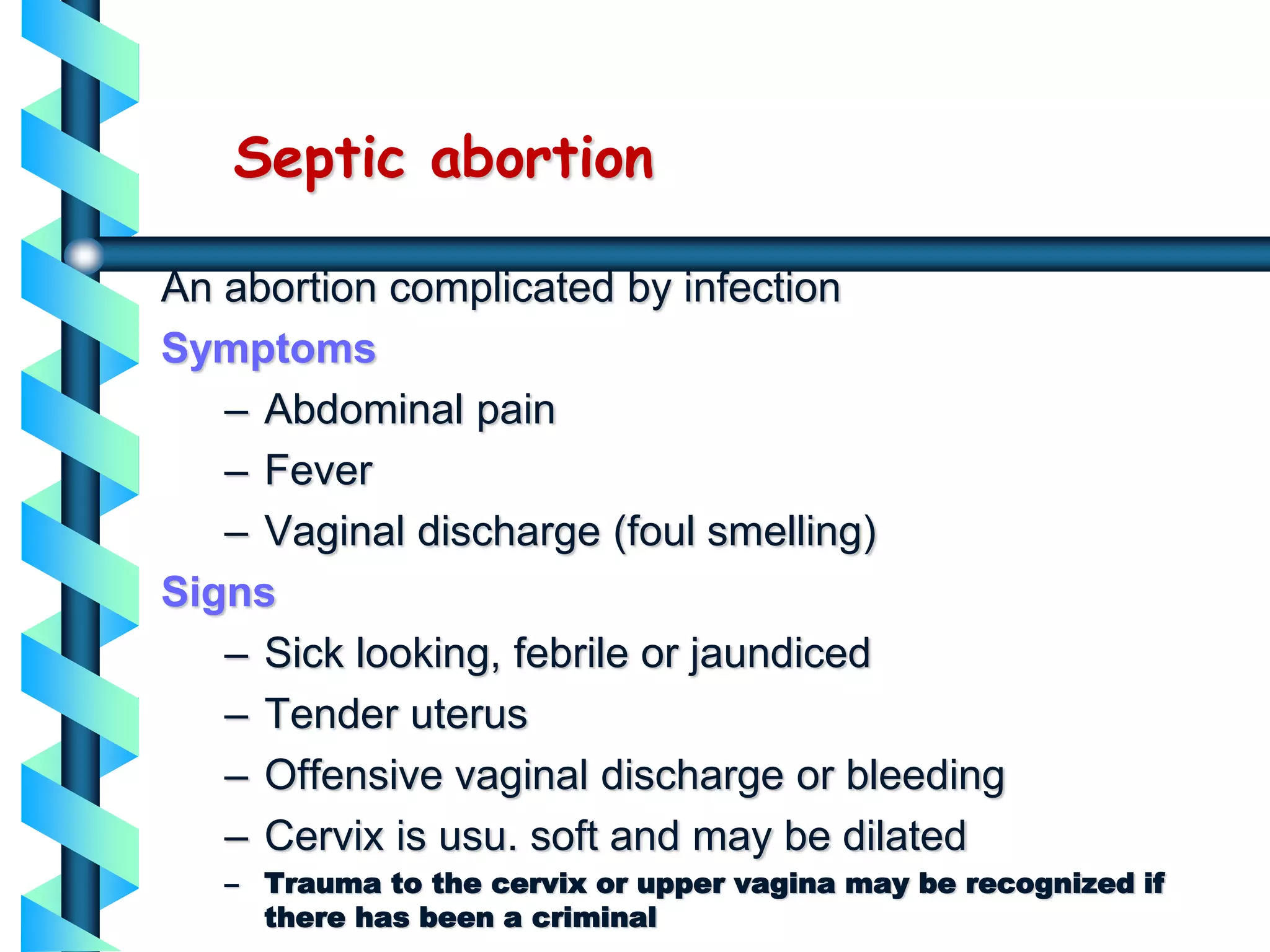
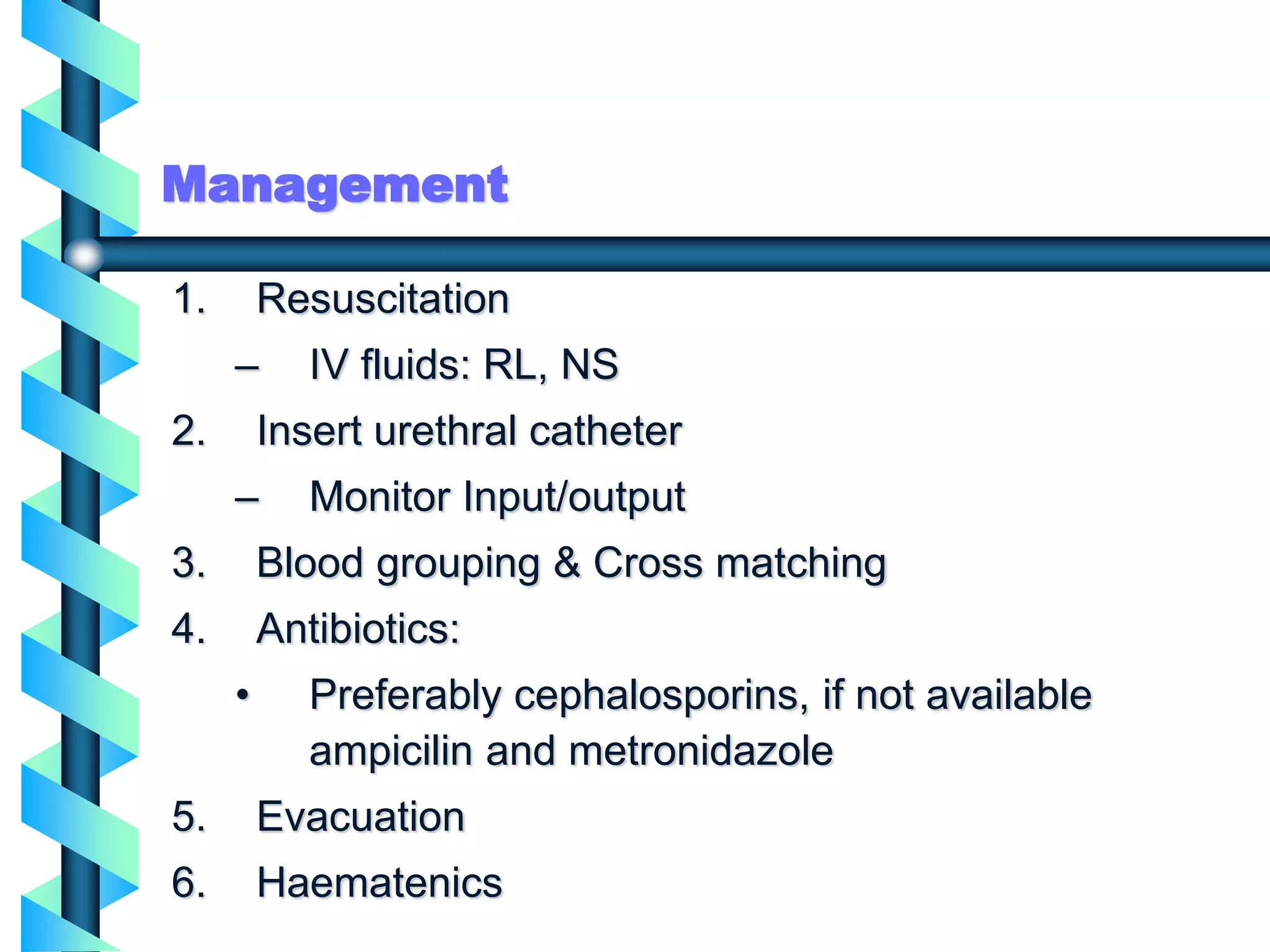
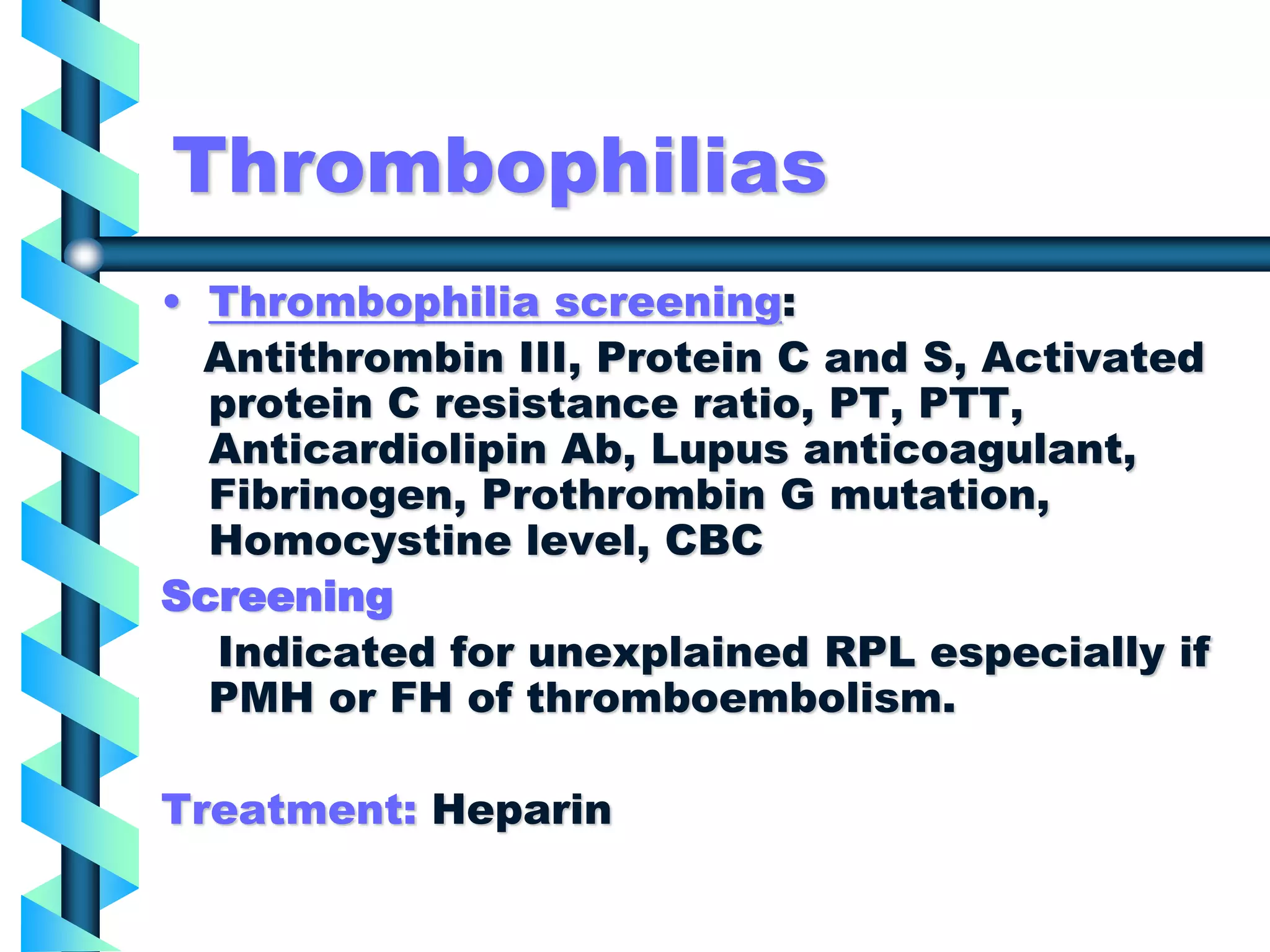
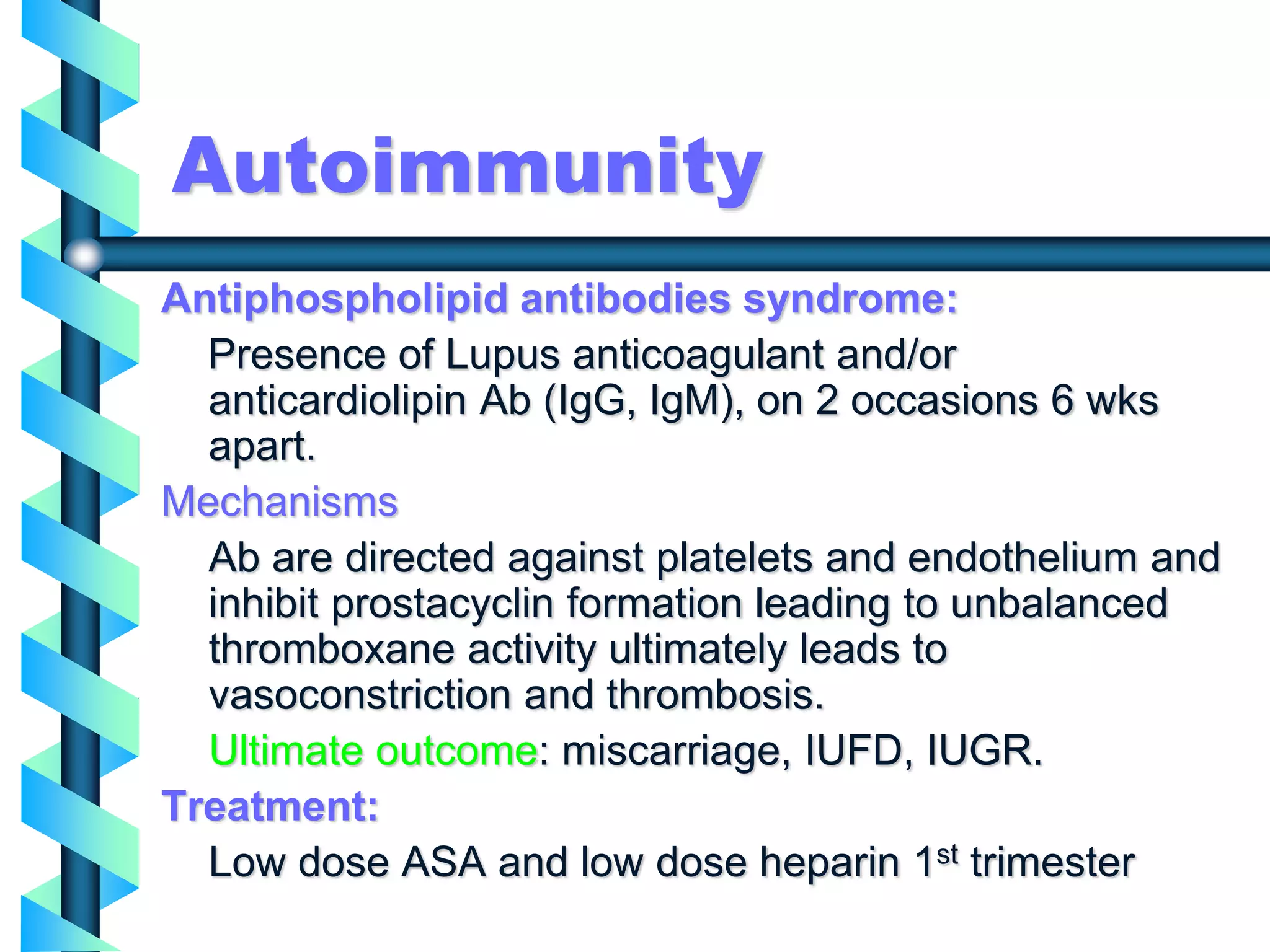
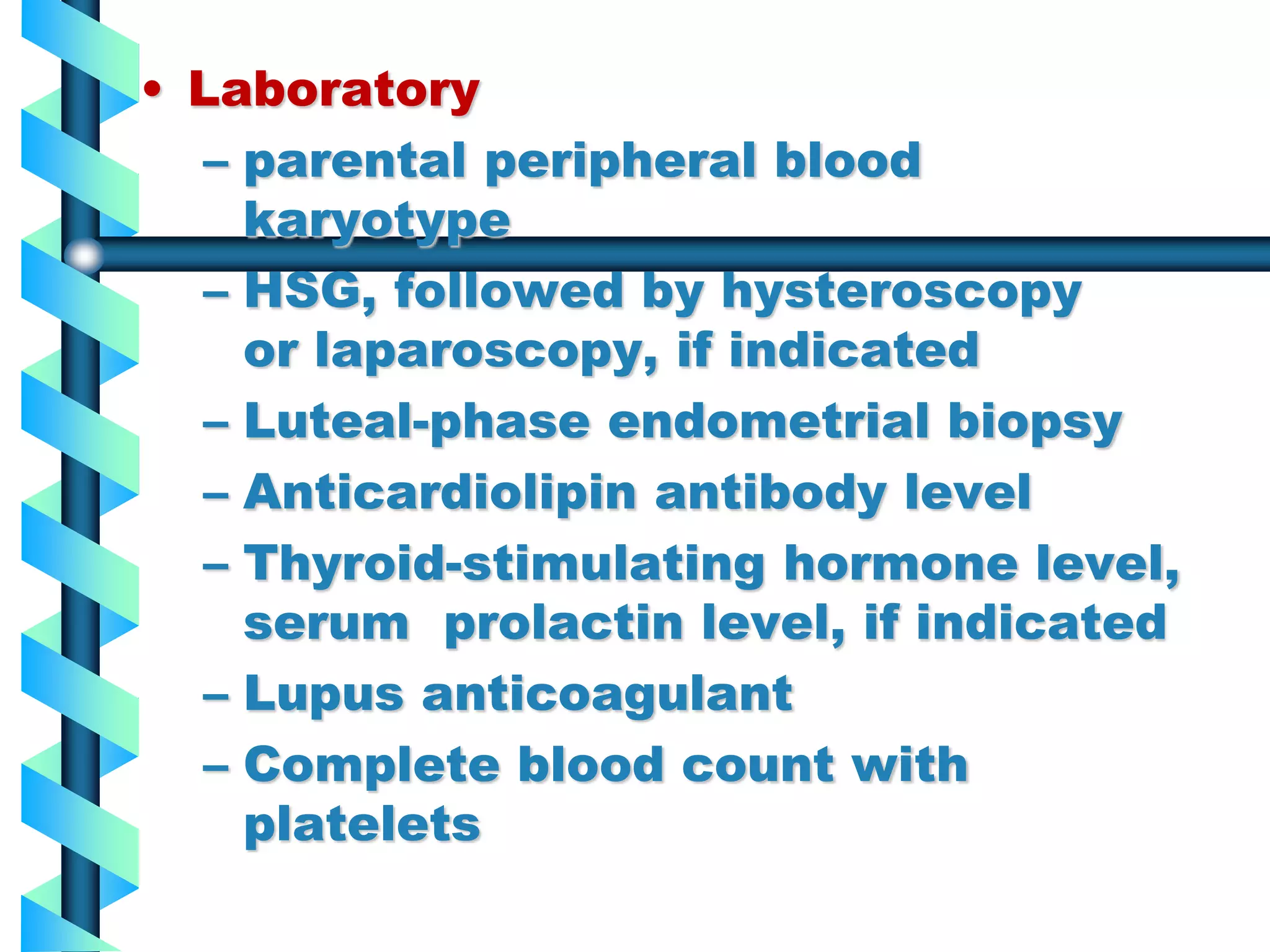
Threatened abortion refers to when the abortion process has started but recovery is still possible. Symptoms include mild pain and bleeding. Inevitable abortion means recovery is no longer possible and symptoms are more severe. Incomplete abortion occurs when some products of conception remain after partial expulsion. Septic abortion is complicated by infection. Recurrent pregnancy losses are defined as 3 or more consecutive losses before 20 weeks and can be caused by genetic, anatomical, endocrine, infectious, thrombotic or immunological factors. Evaluation includes history, exam, labs and testing depending on suspected etiology.