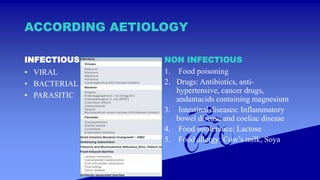
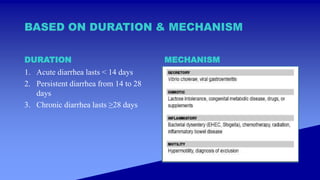
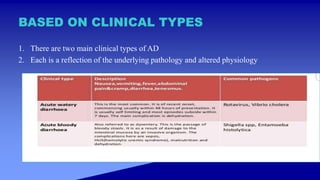
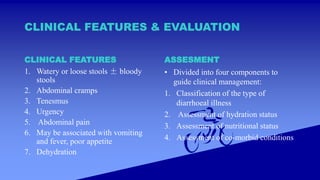
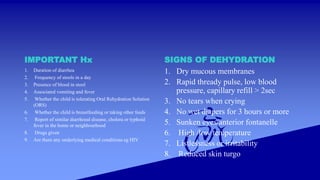
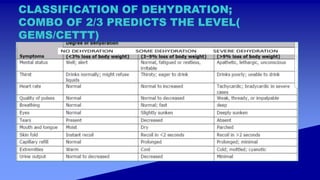
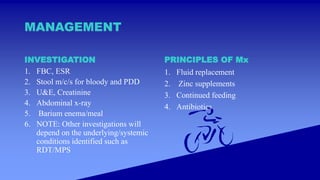
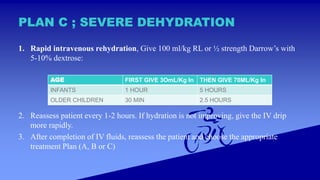
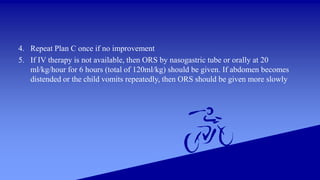
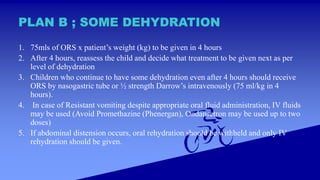
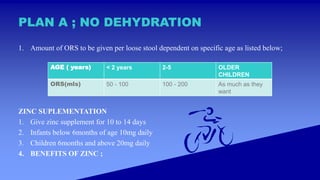
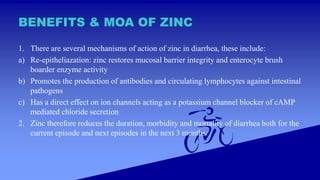
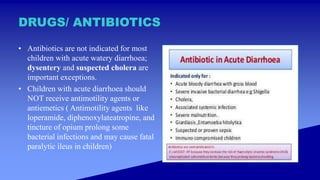
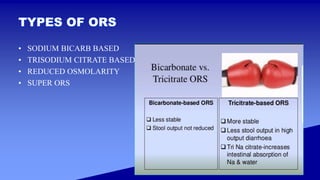
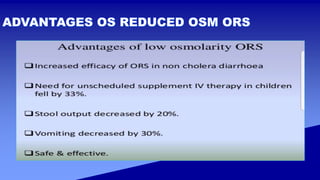
This document discusses acute diarrheal disease, including its definition, classification, risk factors, clinical features, evaluation, and management. It defines acute diarrhea as three or more loose stools per day. It classifies diarrhea based on pathogens, duration, and mechanism. Risk factors include young age, immune deficiency, malnutrition, and exposure to unsanitary conditions. Clinical assessment involves classifying the illness, assessing hydration and nutritional status, and looking for comorbidities. Management involves fluid replacement, zinc supplementation, continued feeding, and antibiotics in some cases. The principles of rehydration therapy are outlined depending on the level of dehydration.