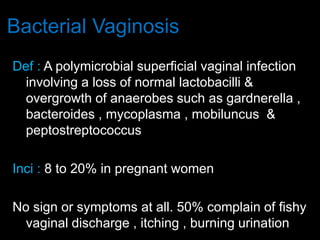
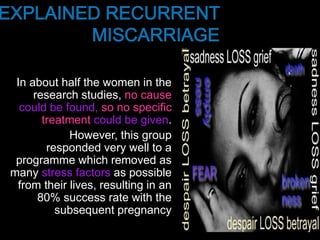
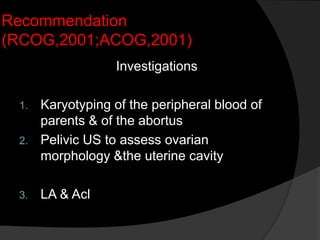
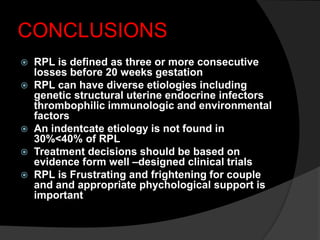
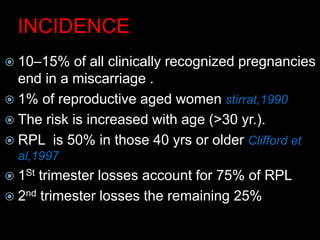
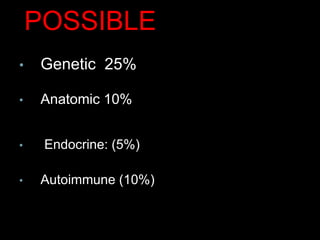
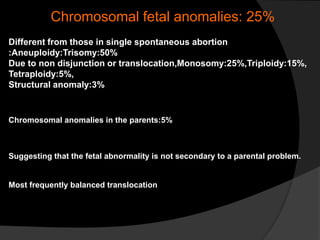
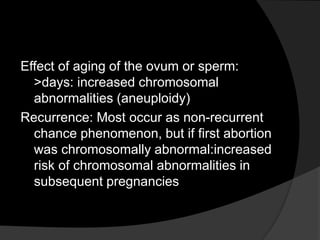
Recurrent pregnancy loss is defined as 3 or more consecutive pregnancies ending in spontaneous abortion before 20 weeks. The causes of recurrent pregnancy loss can be established in only 30-50% of cases and include genetic abnormalities, anatomic abnormalities of the uterus, endocrine disorders, autoimmune conditions, infections, and environmental factors. While extensive testing and treatments are available, the cause remains unidentified in 30-40% of recurrent pregnancy loss cases. Providing psychological support to couples experiencing recurrent pregnancy loss can help improve future pregnancy outcomes.
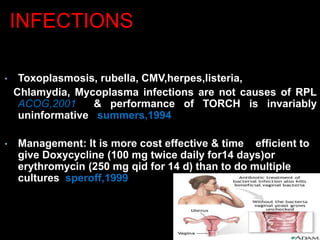
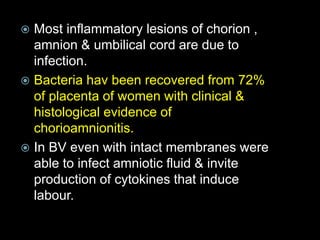
![ TORCH (toxoplasmosis rubella,
cytomegalovirus and herpes simplex virus),
other [congenital syphilis and viruses],
screening is unhelpful in the investigation
of recurrent miscarriage.
For an infective agent to be implicated in the
etiology of repeated pregnancy loss, it must be
capable of persisting in the genital tract and
avoiding detection or must cause insufficient
symptoms to disturb the women.
Toxoplasmosis, rubella, cytomegalovirus,
herpes and listeria infections do not fulfil these
criteria and routine TORCH screening should
be abandoned.](https://image.slidesharecdn.com/impactoftheproblem-171117123330/85/Recurrent-Pregnancy-Loss-33-320.jpg)