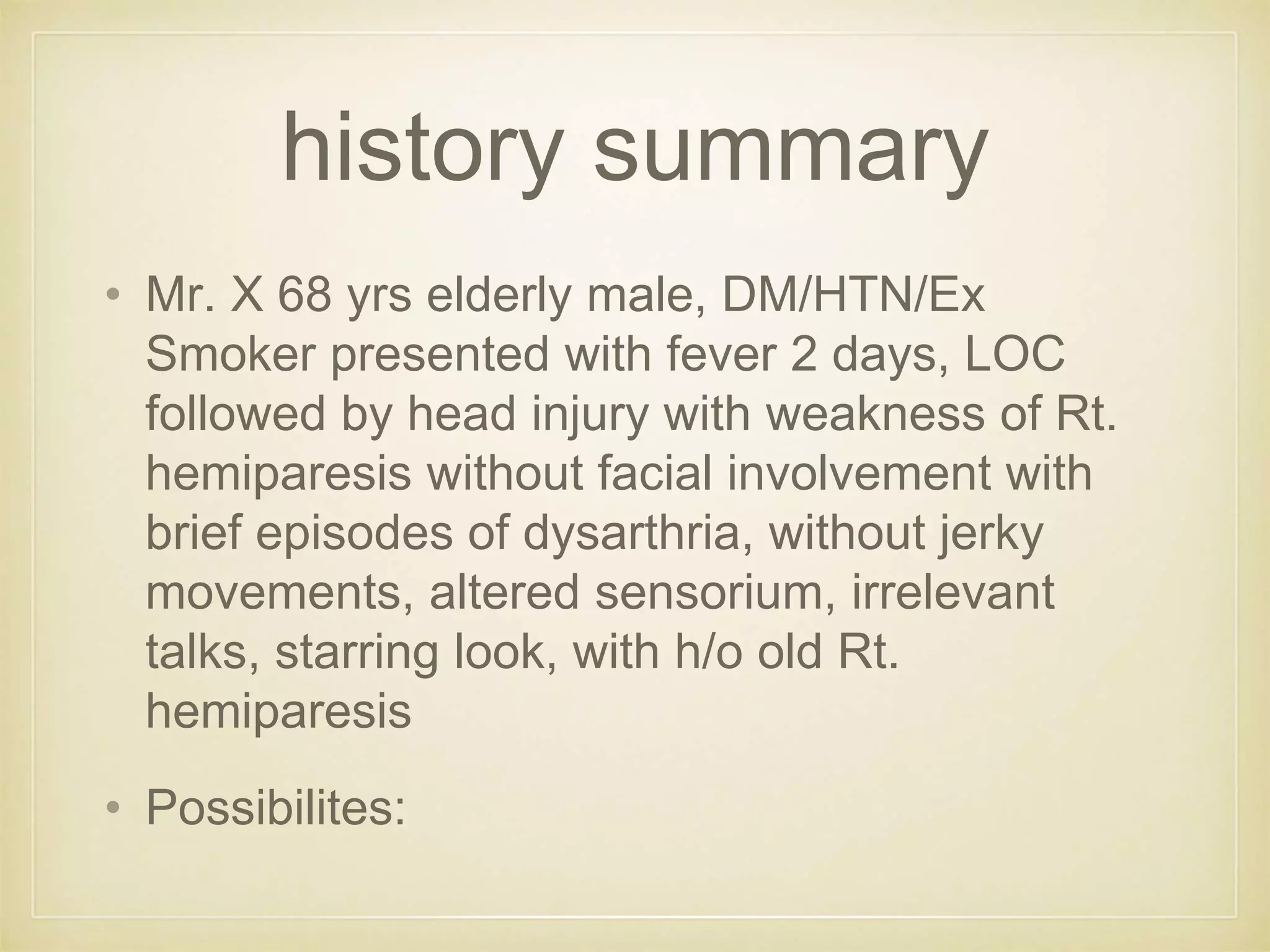
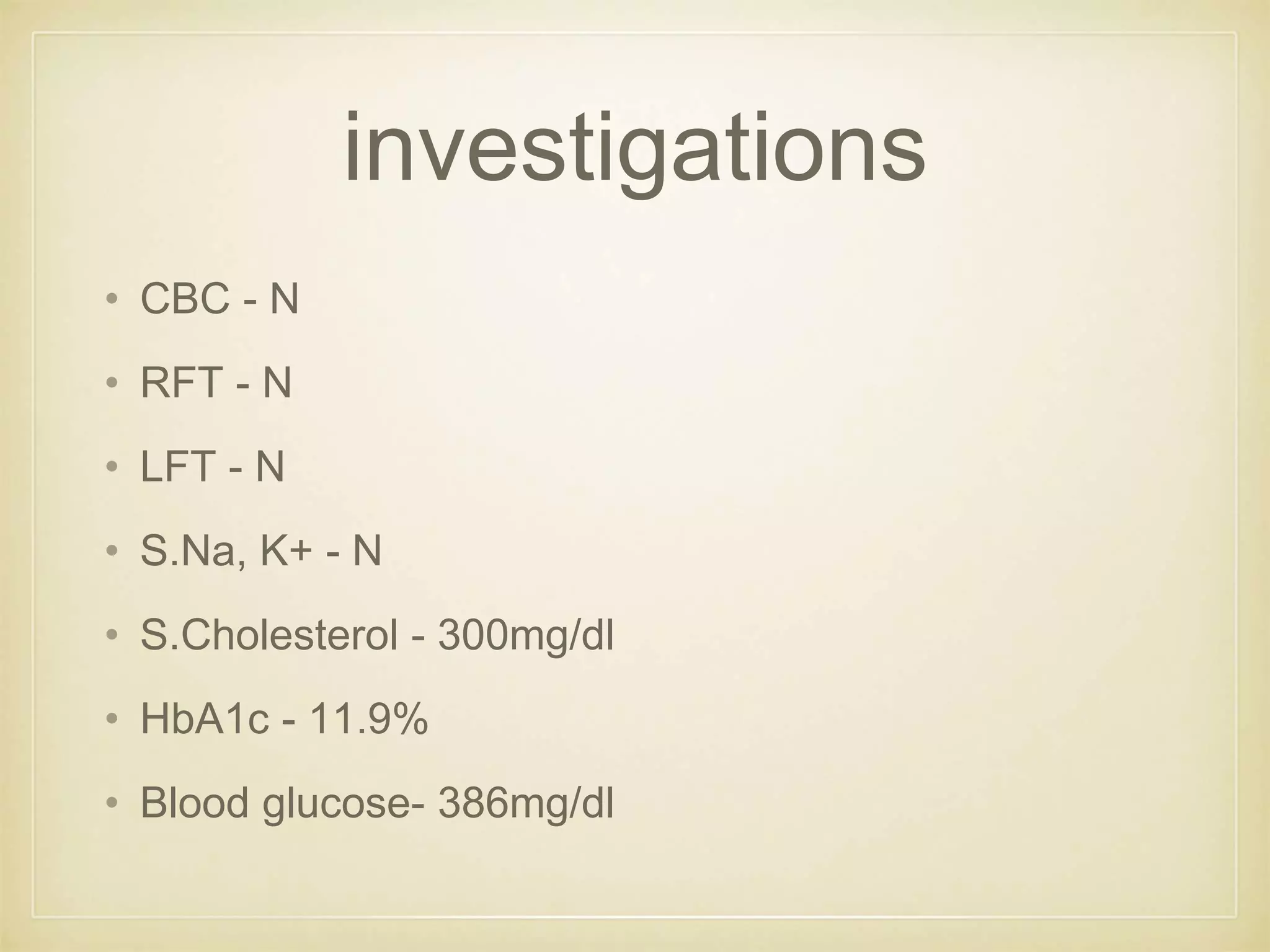
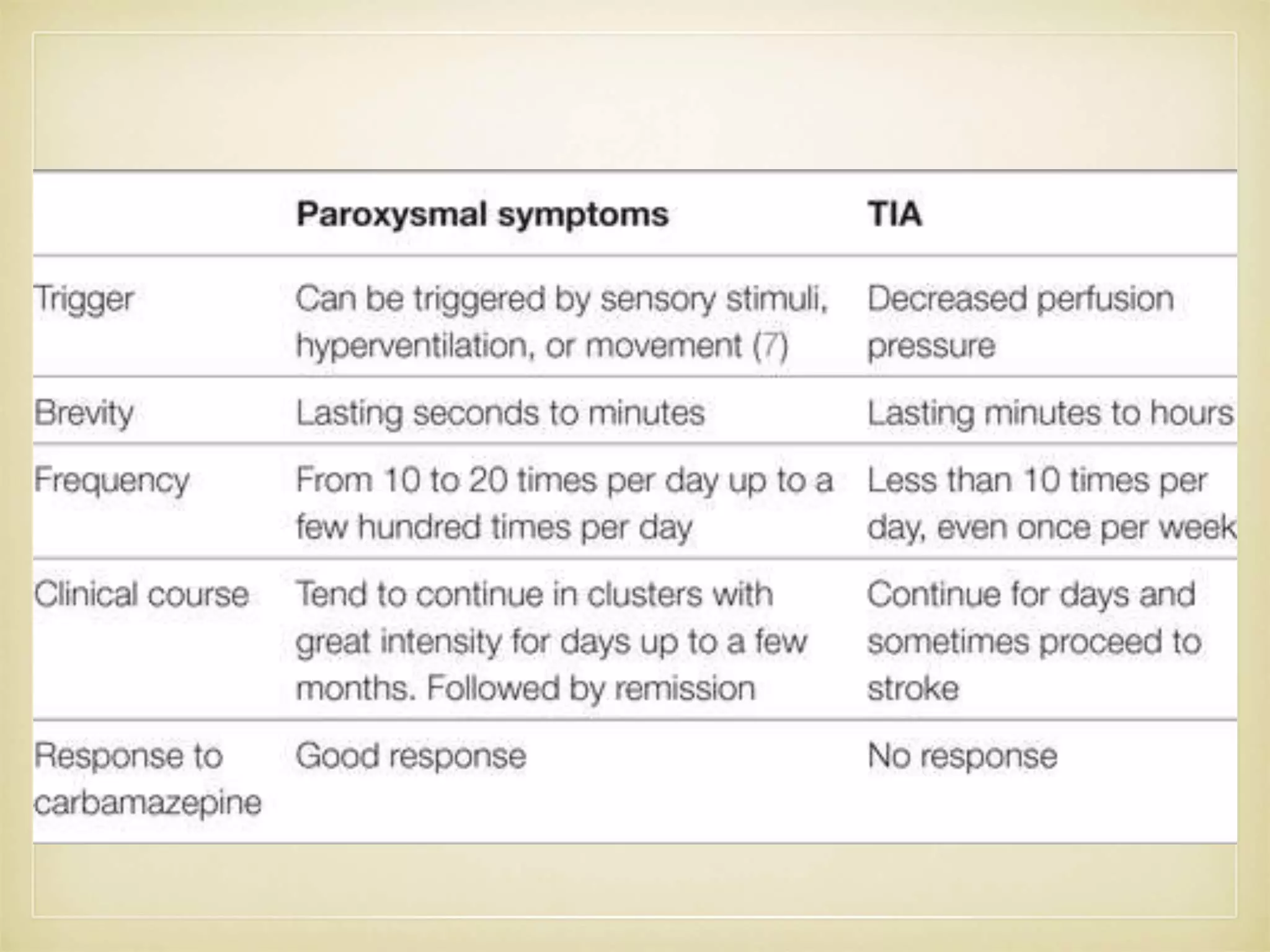
This document presents the case of a 68-year-old male who presented with fever and loss of consciousness followed by a fall and weakness on his right side. He experienced brief episodes of dysarthria lasting 5-10 minutes associated with swallowing difficulty. Imaging showed a subdural hematoma in the right frontal-temporal-parietal region. He was treated and improved but later experienced paroxysmal dysarthria again, which was controlled with anti-seizure medication. The causes and potential mechanisms of his paroxysmal dysarthria are discussed.