The document discusses various topics related to neurology including:
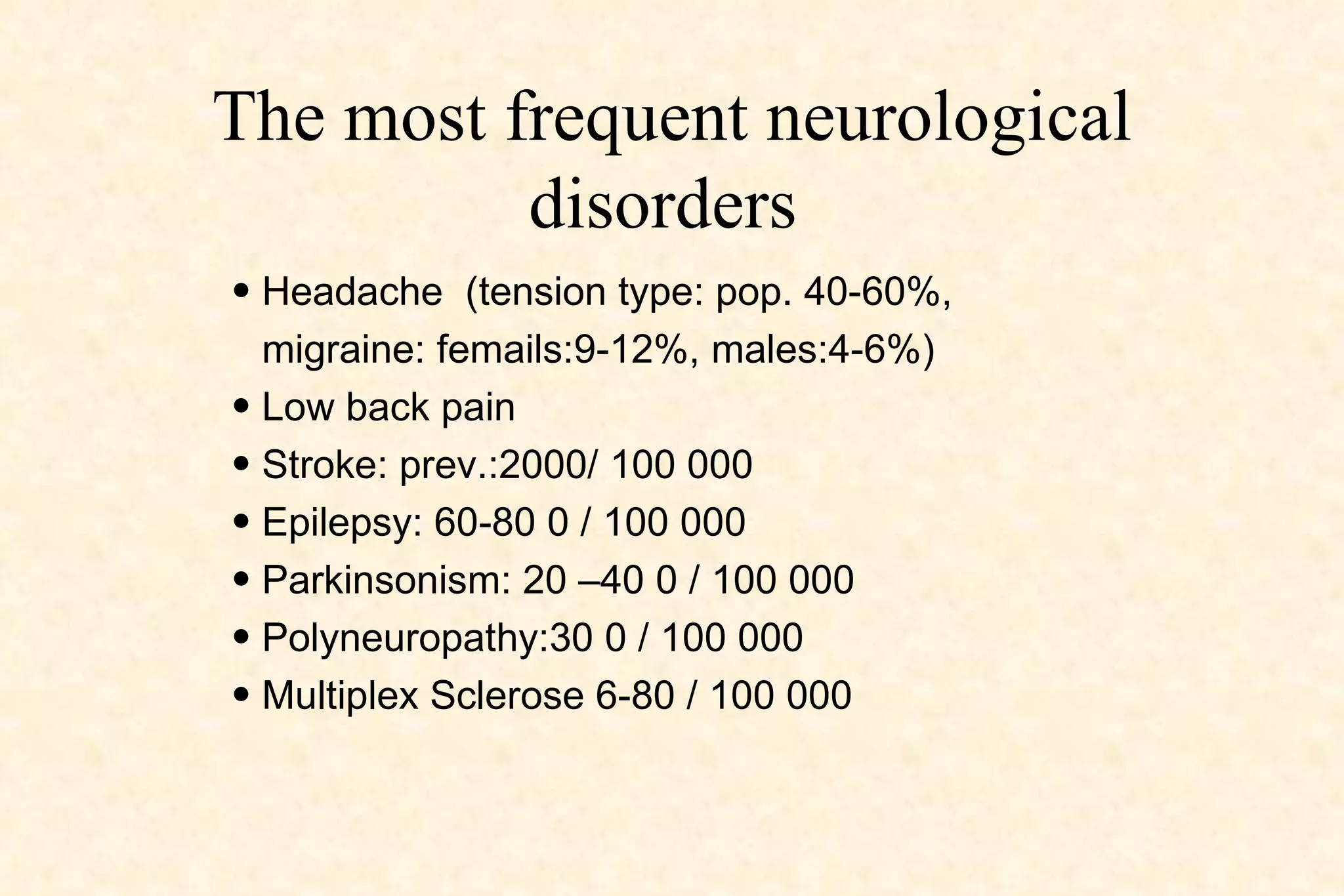
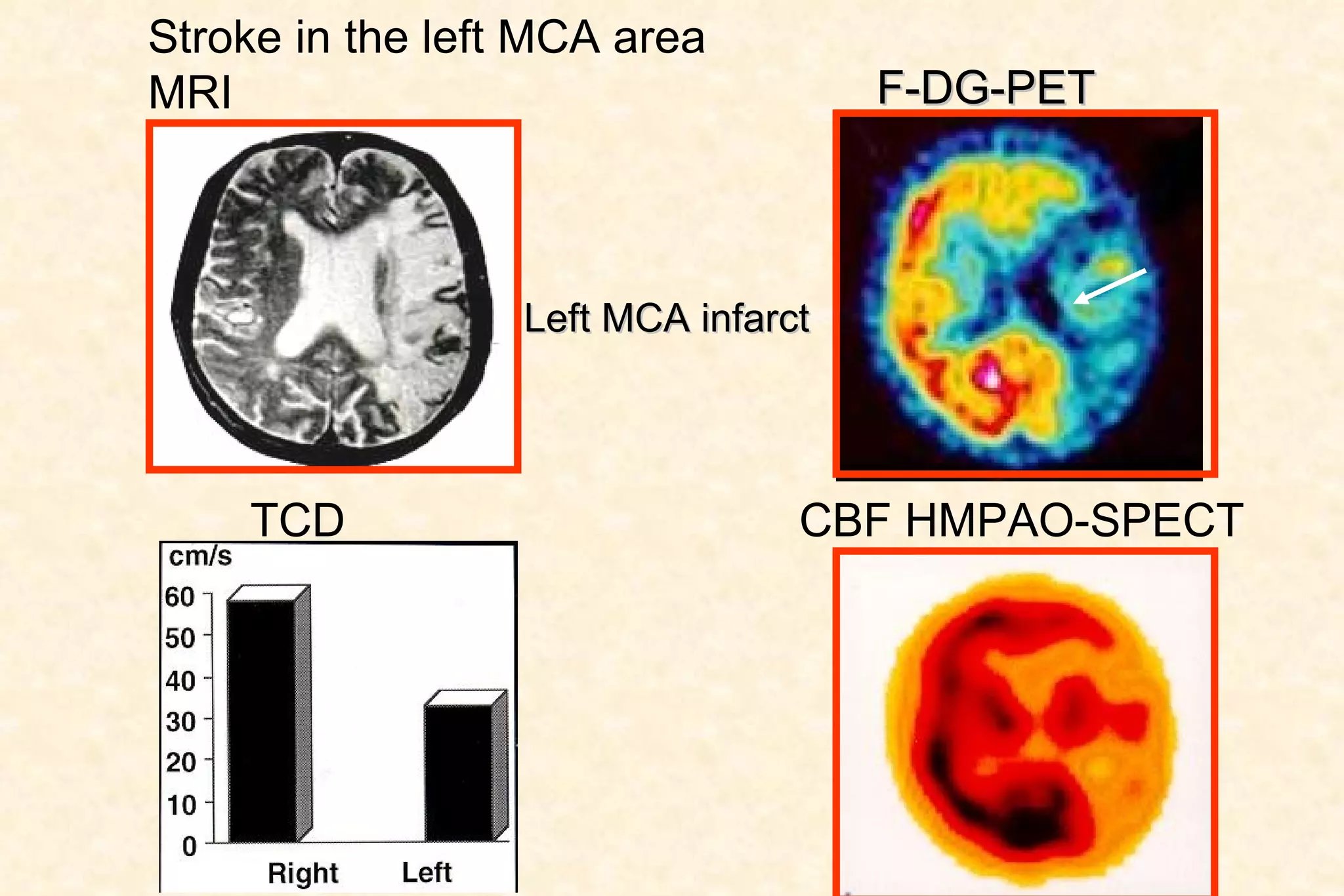
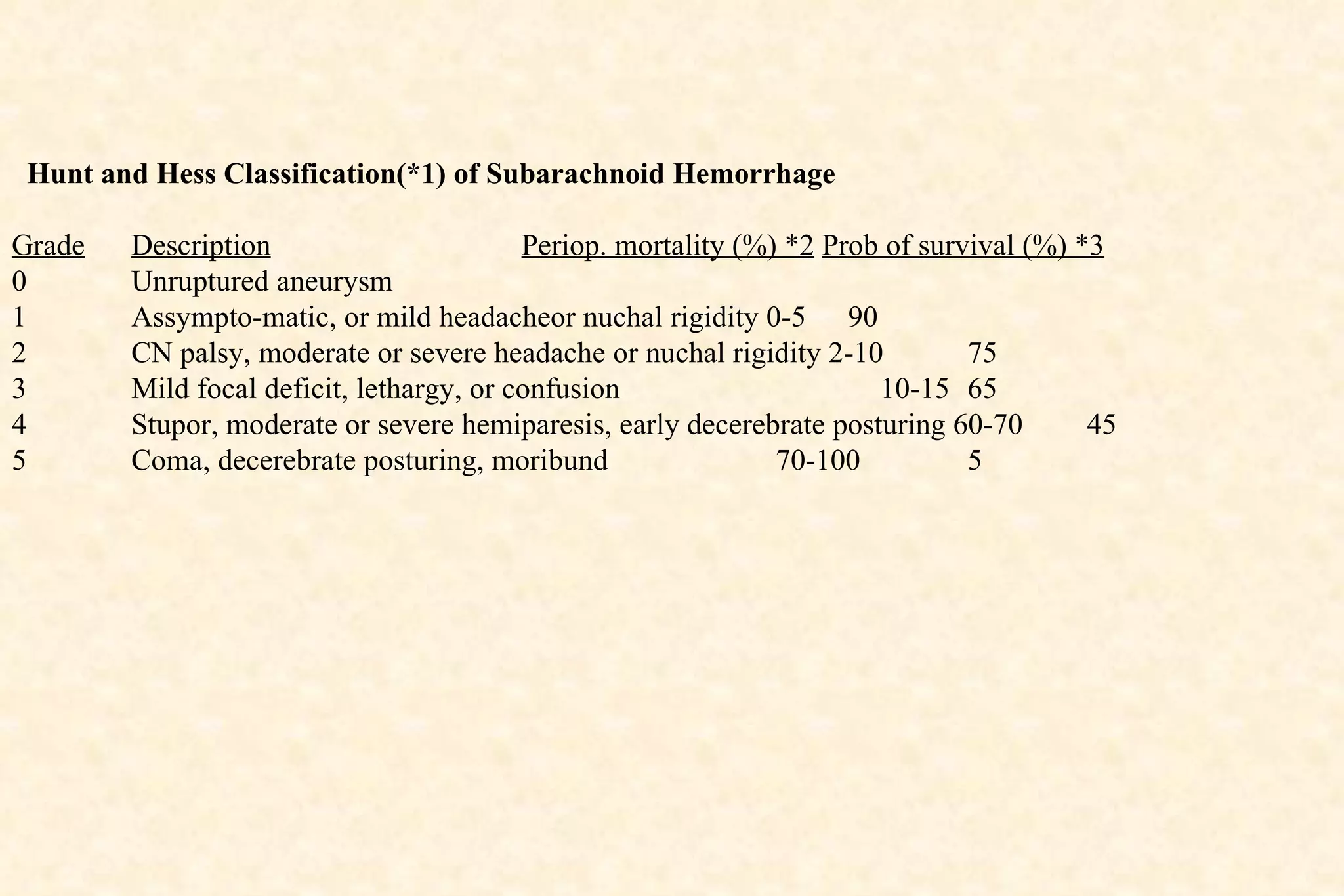
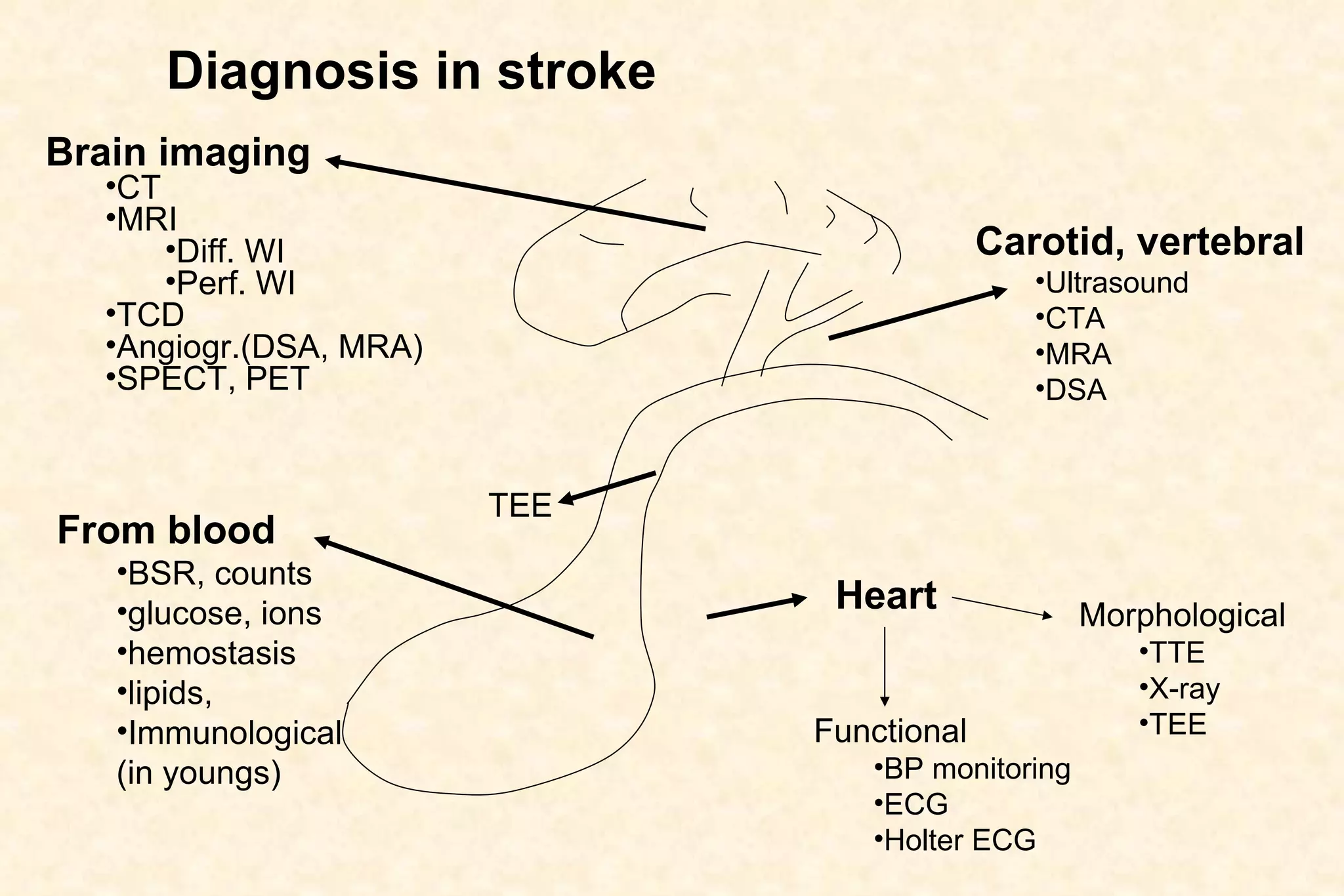
1. Common neurological disorders such as headache, low back pain, and stroke.
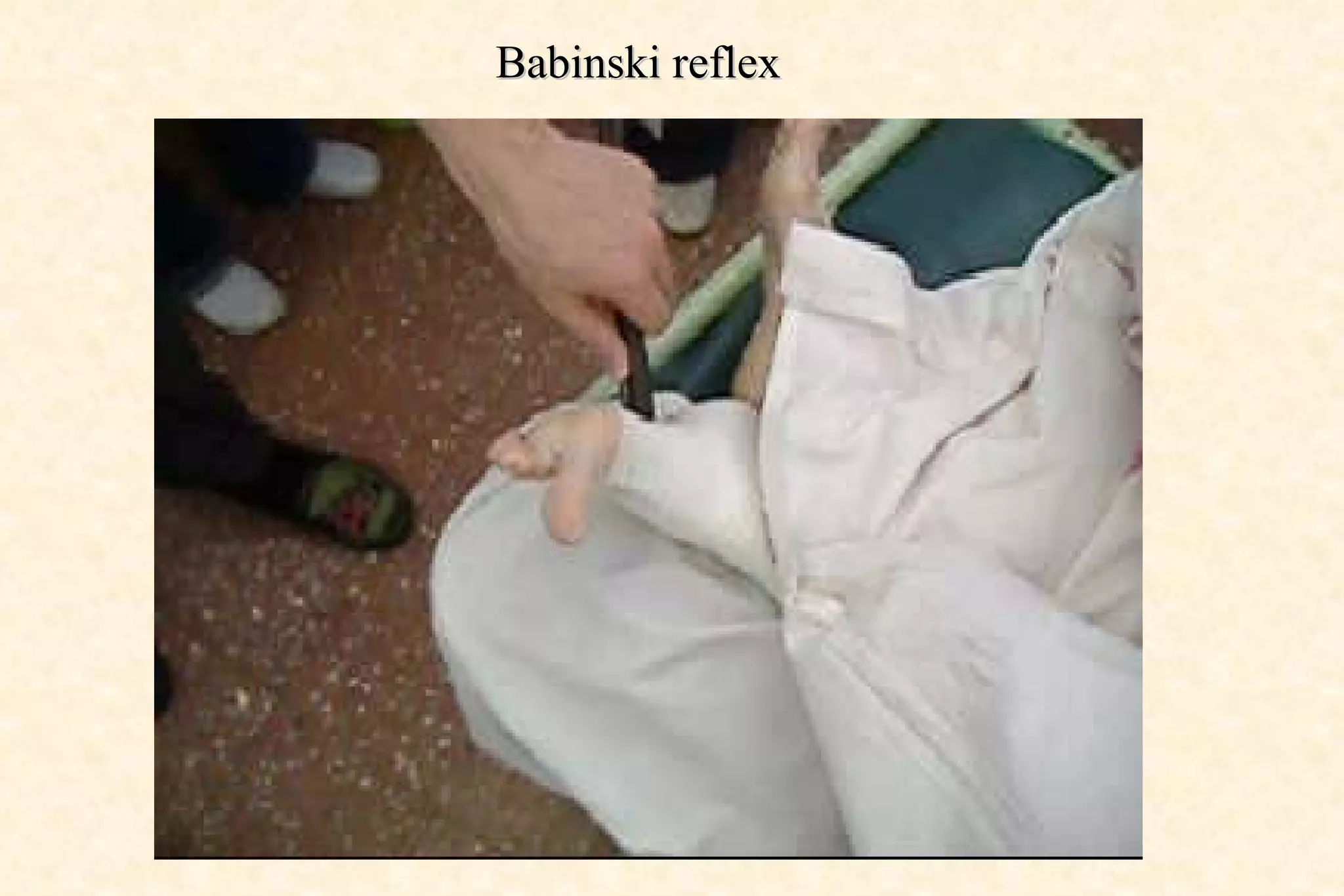
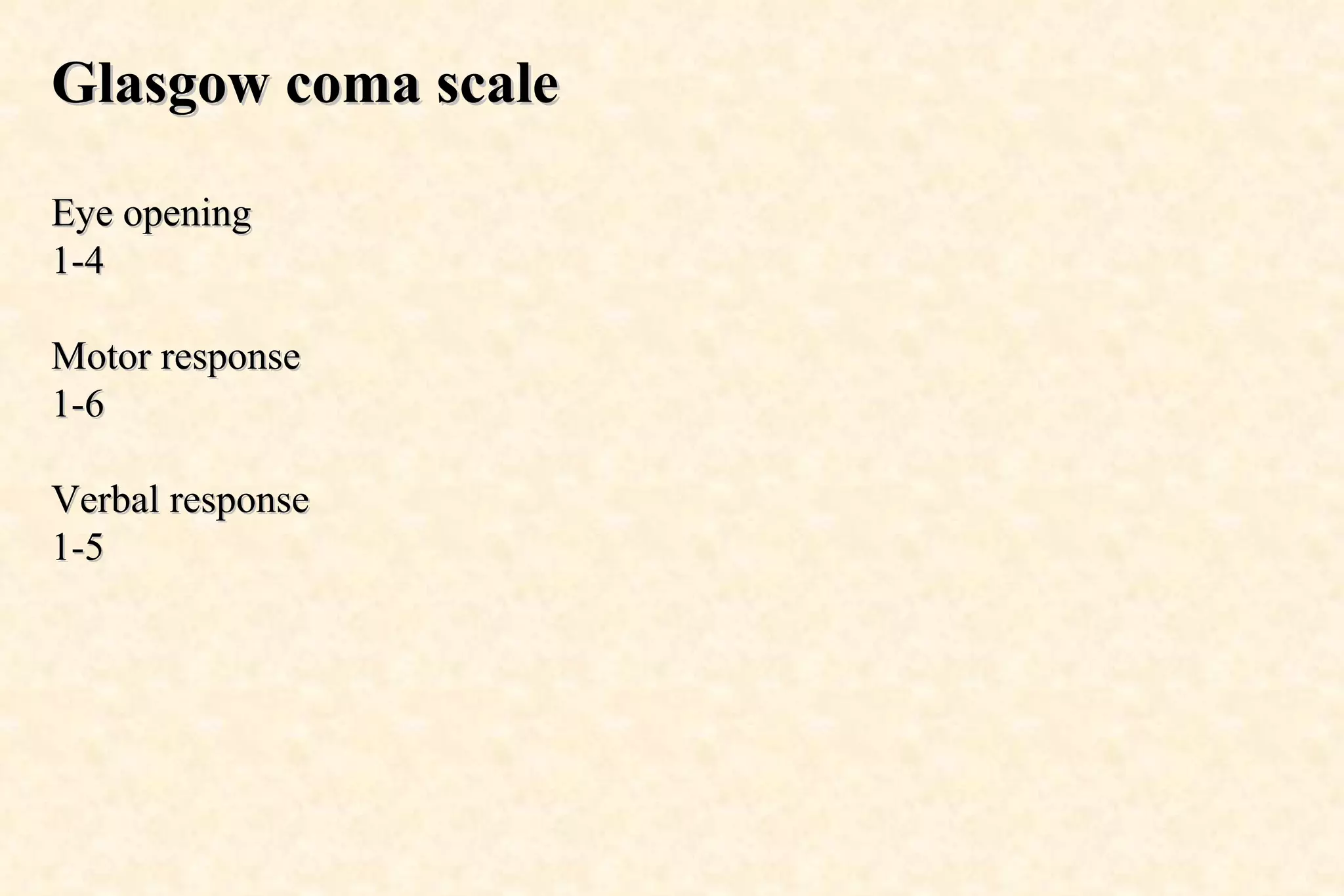
2. Components of a neurological examination including signs, reflexes, and tests of sensory and motor function.
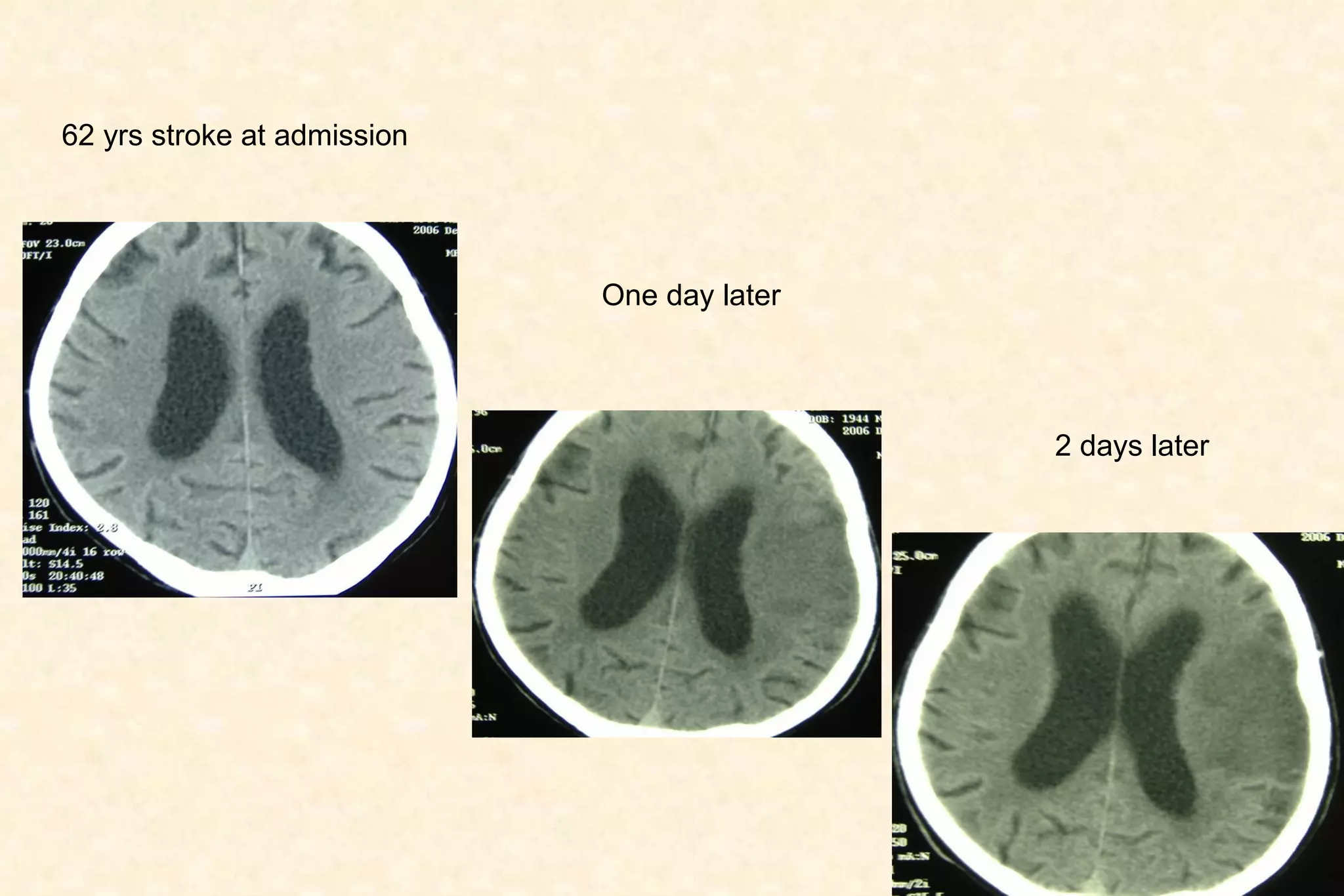
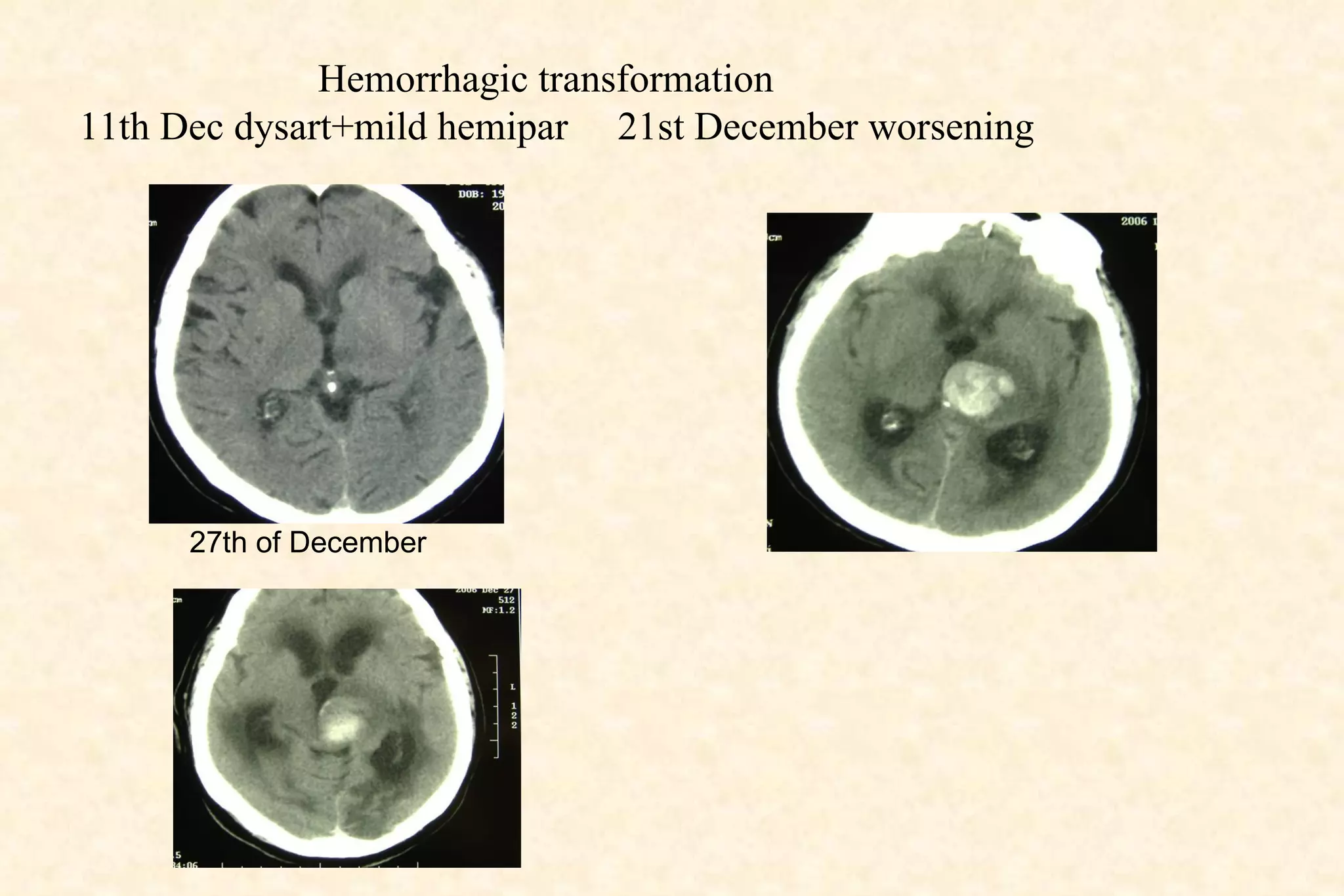
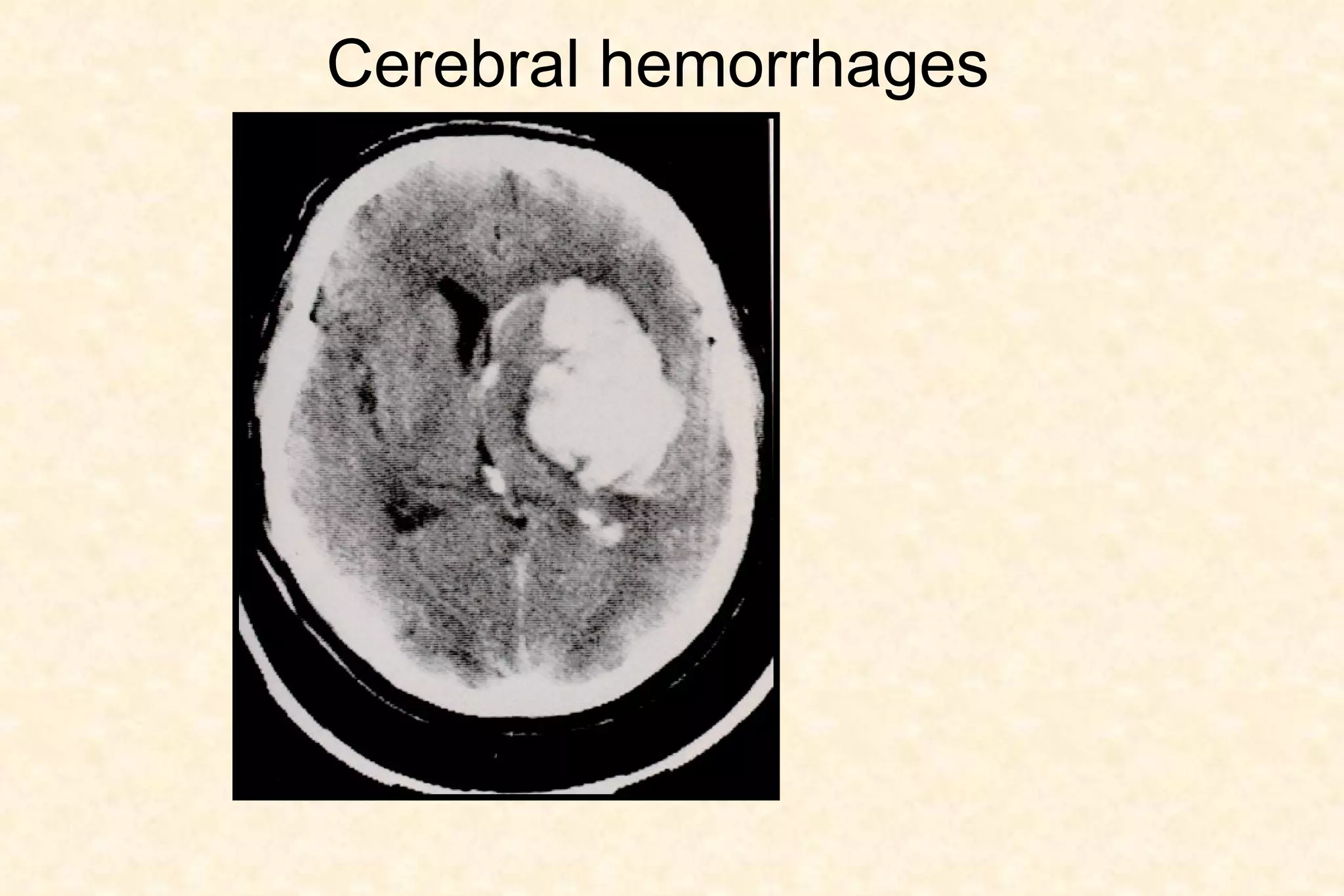
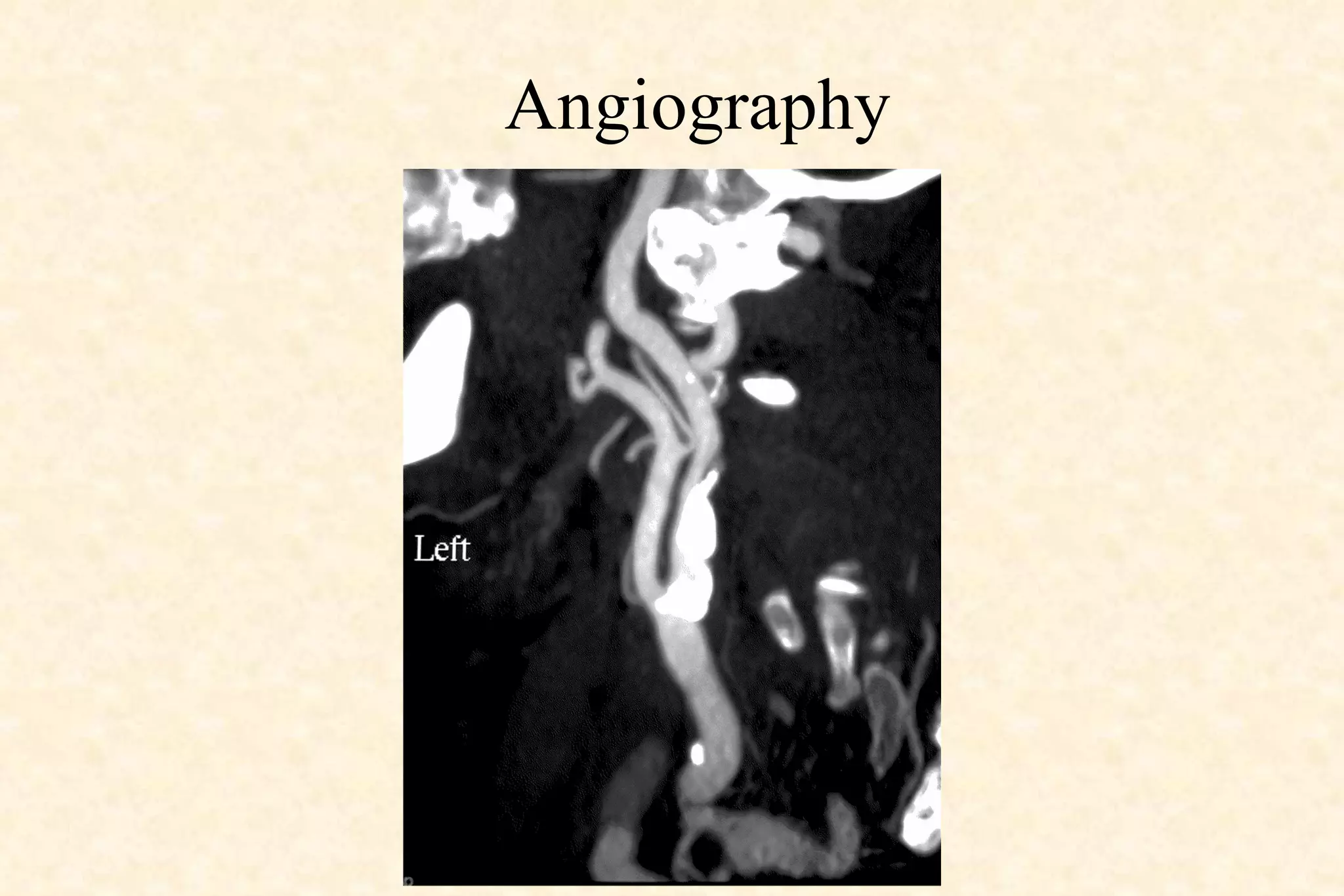
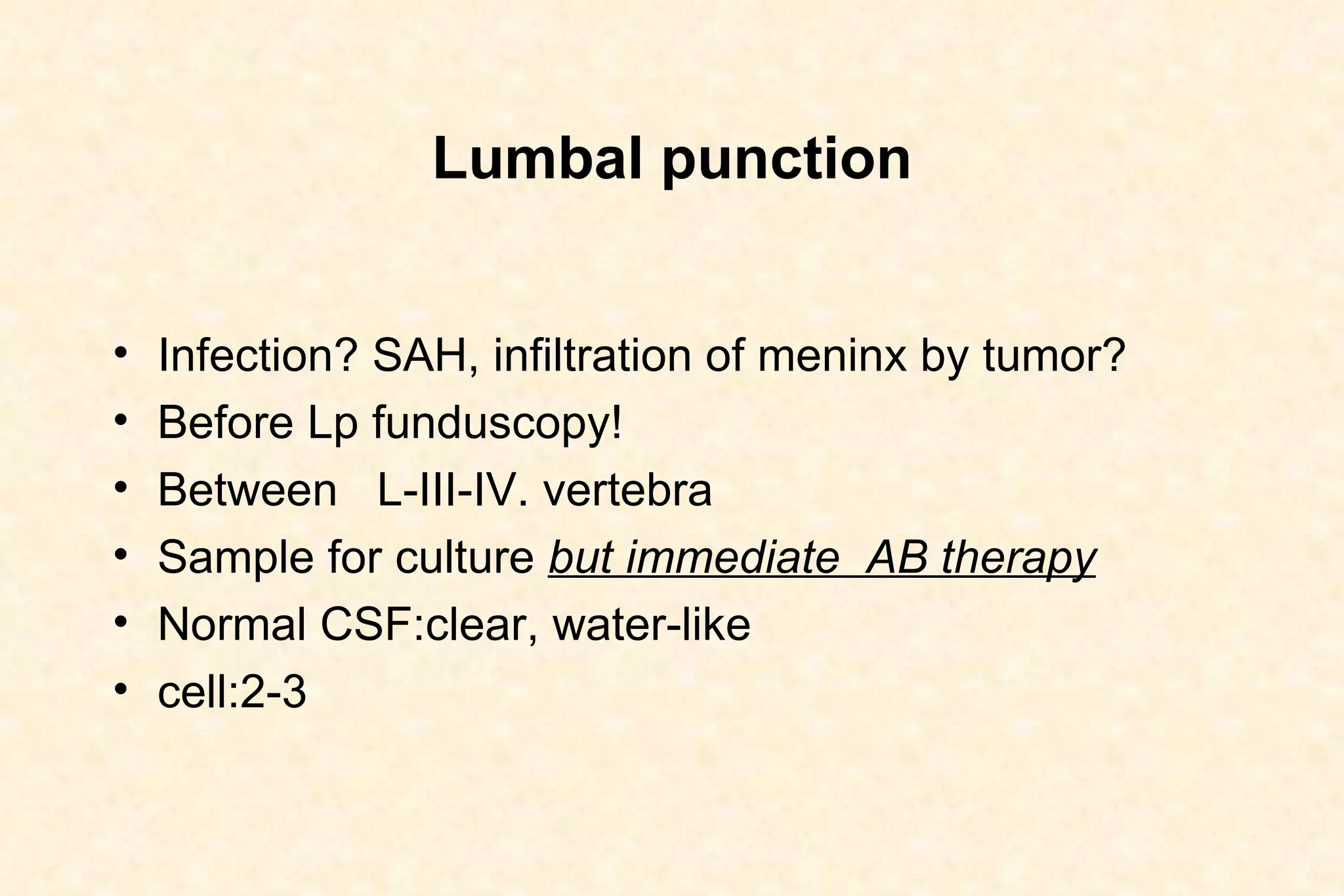
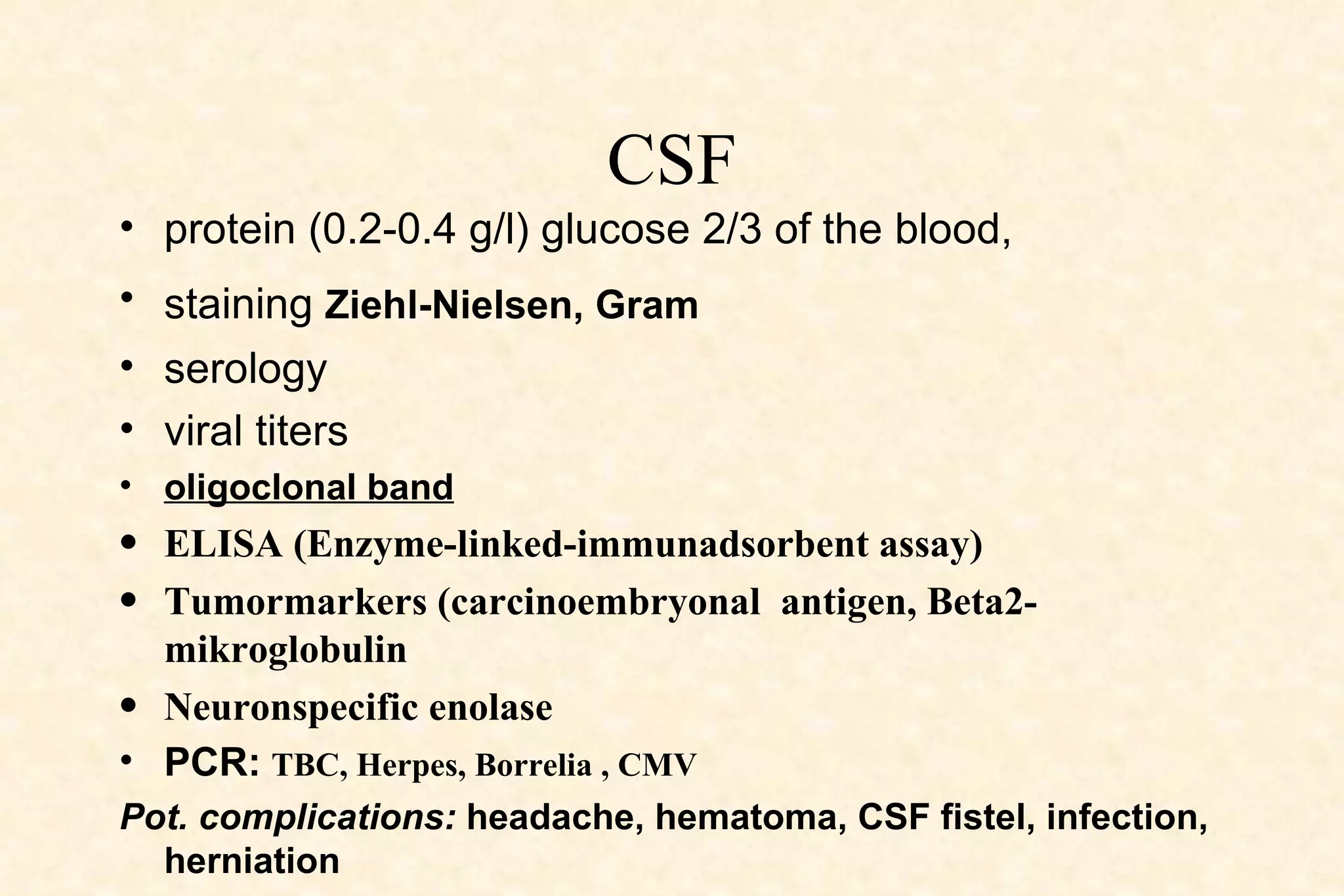
3. Diagnostic tools used in neurology such as CT, MRI, angiography, EEG, lumbar puncture, and PET.
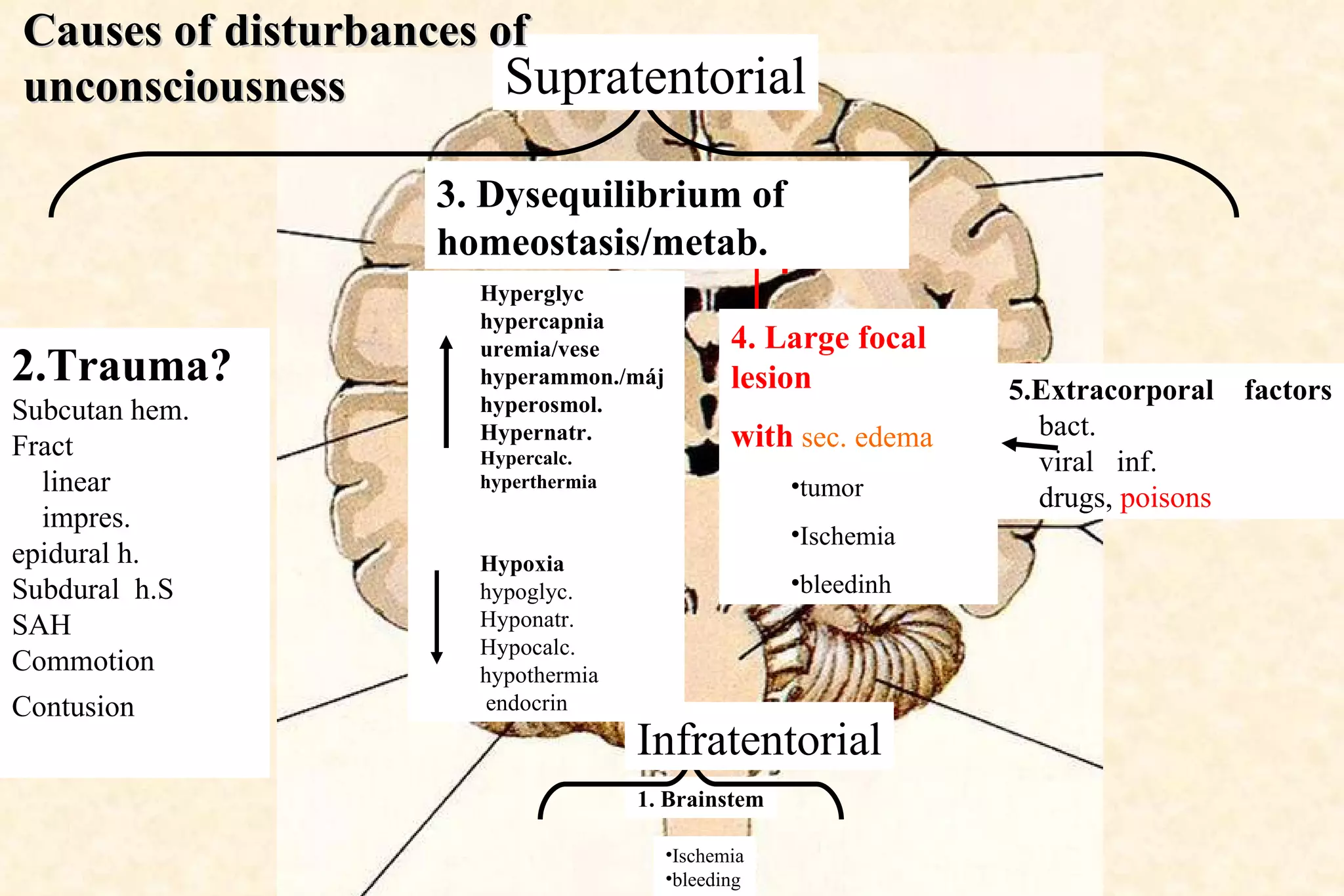
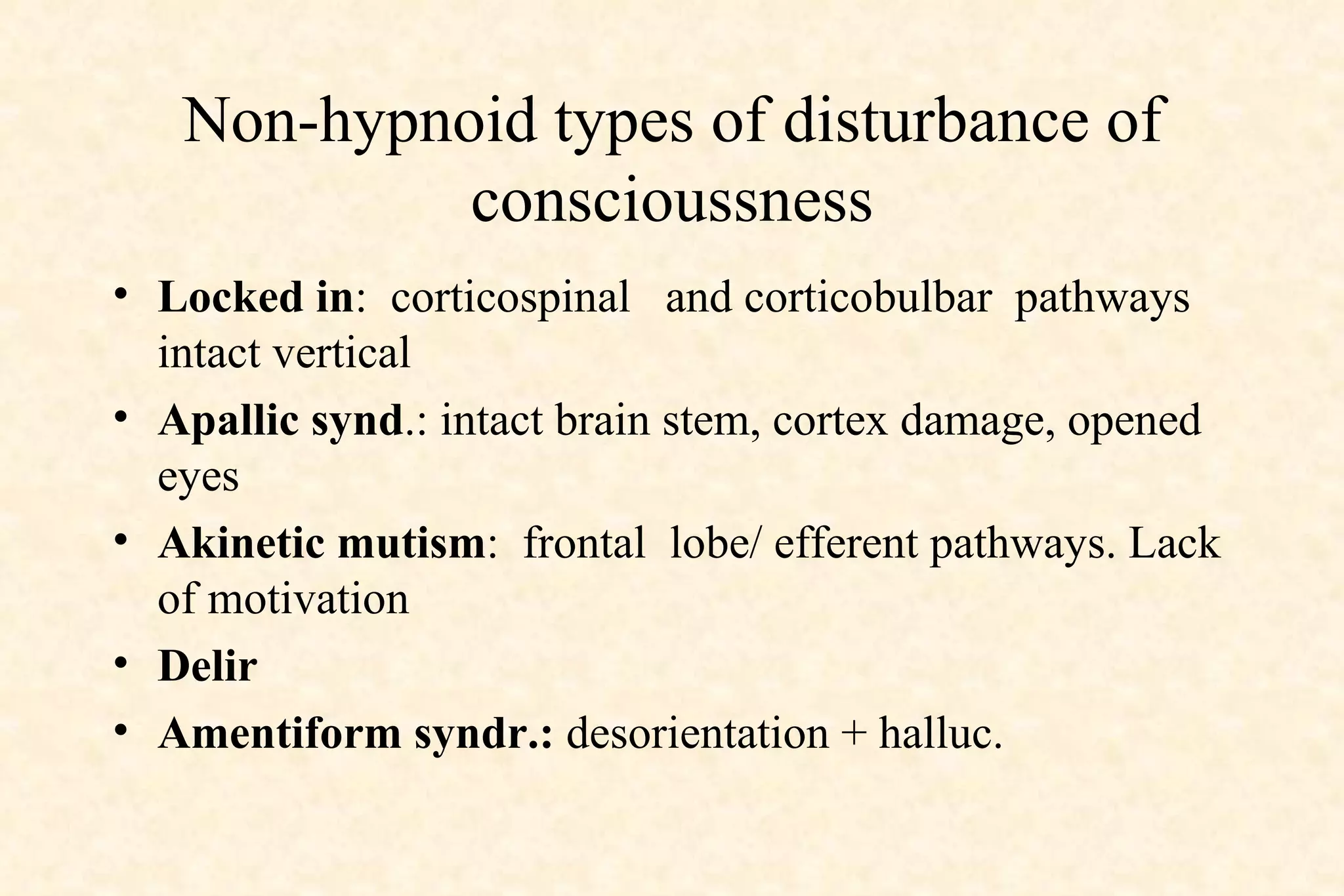
4. Types of disturbances of consciousness including those caused by brainstem or cortical damage.
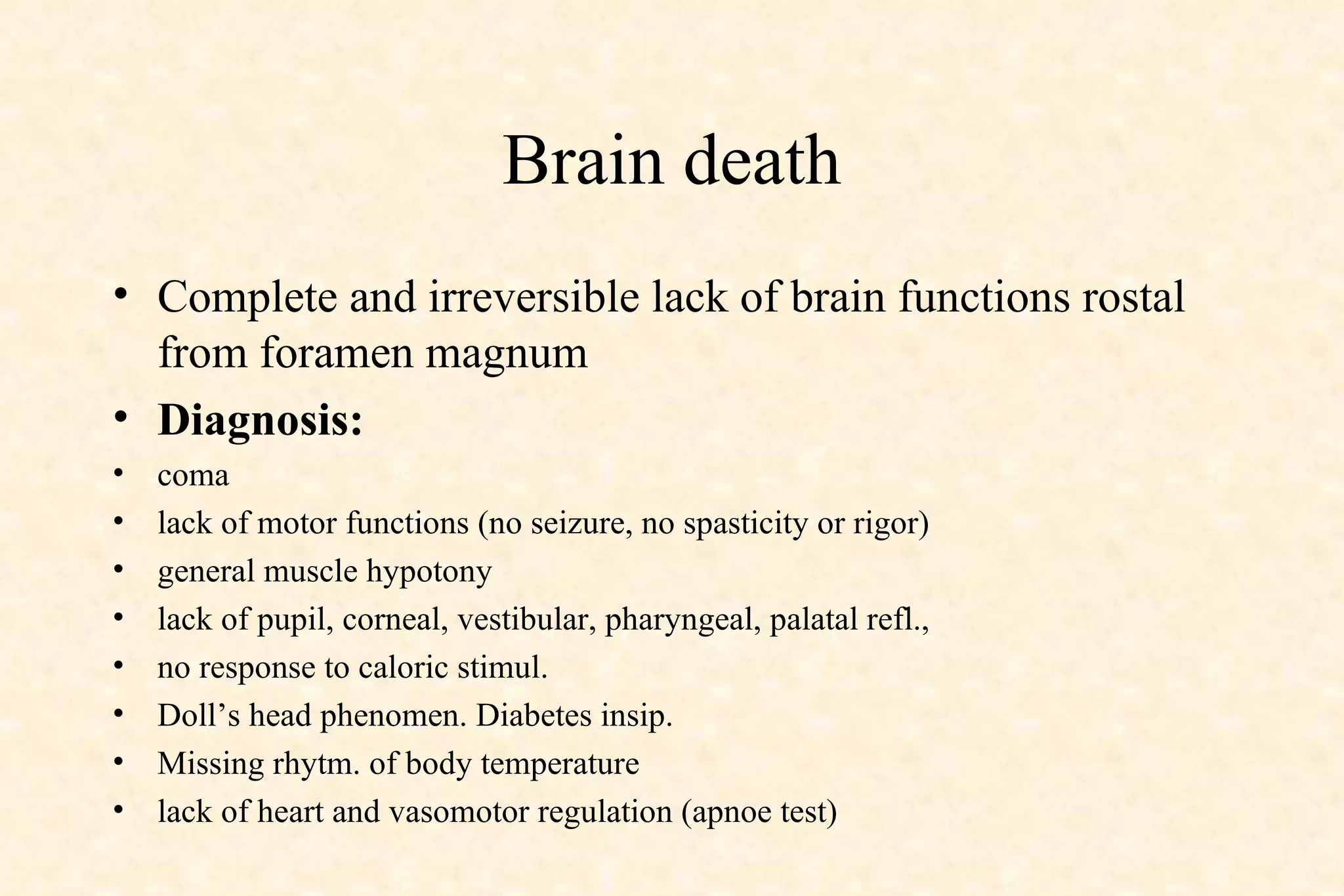
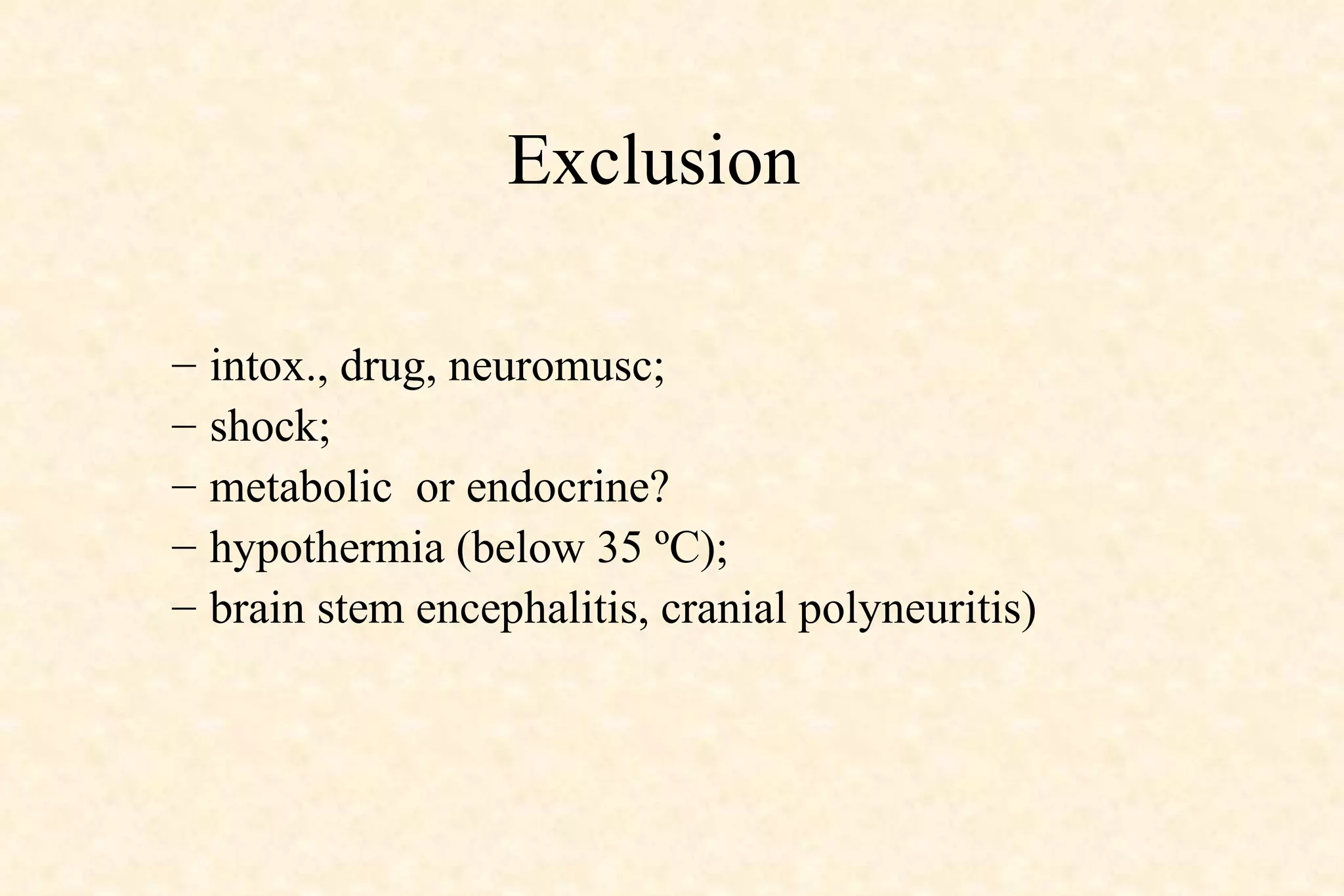
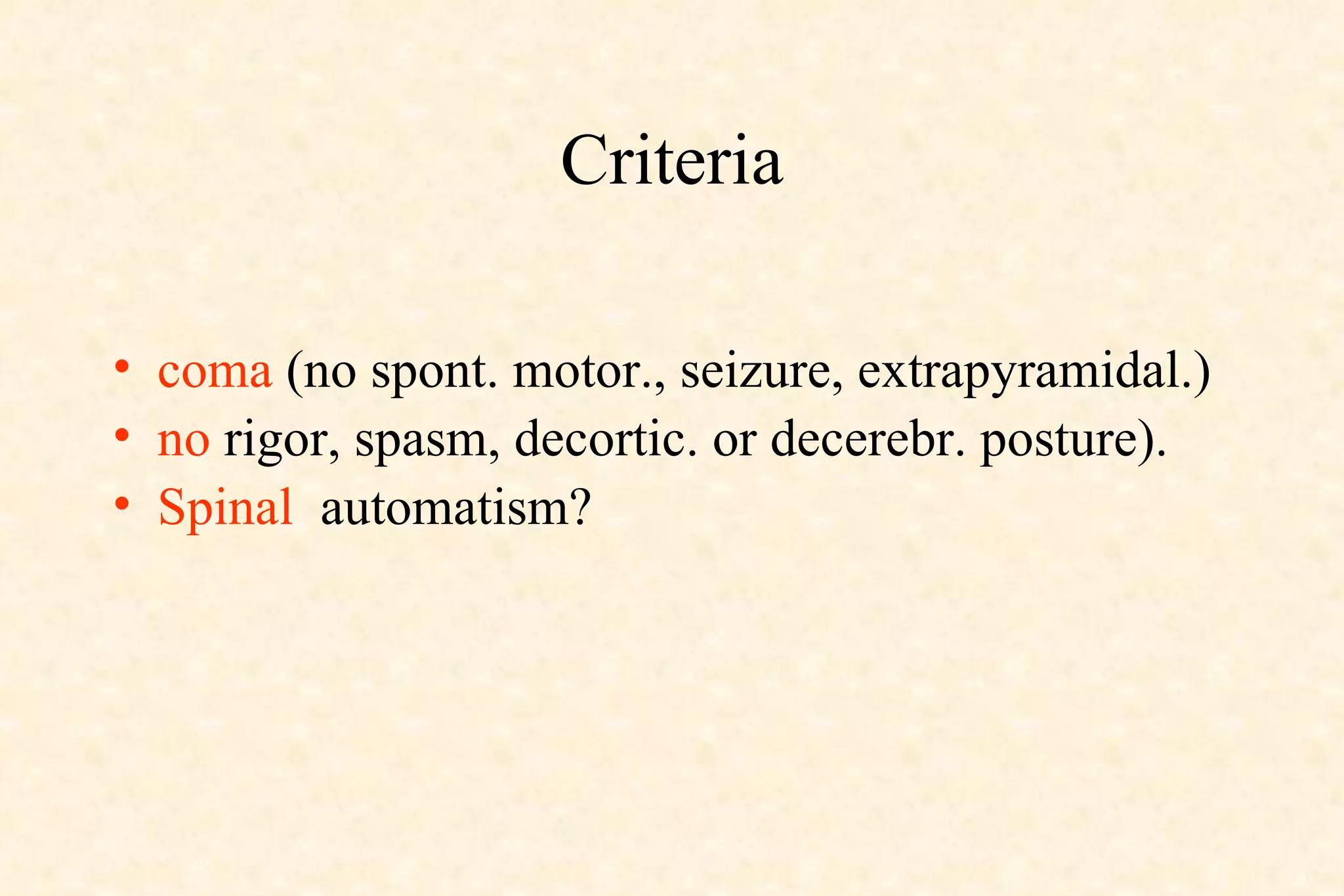
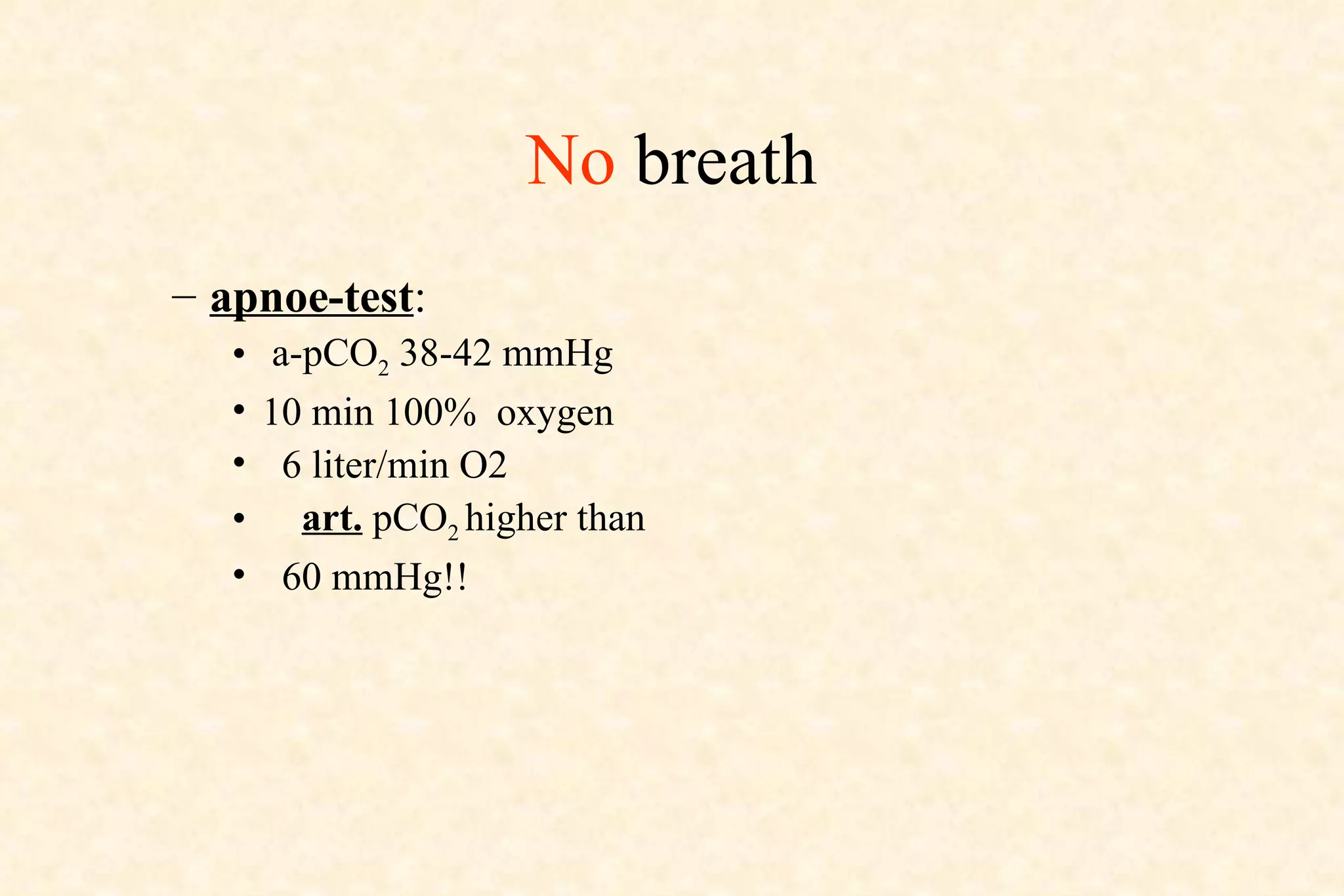
5. Criteria for determining brain death.