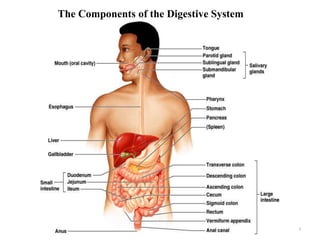
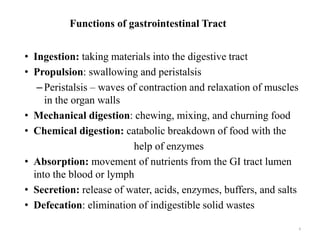
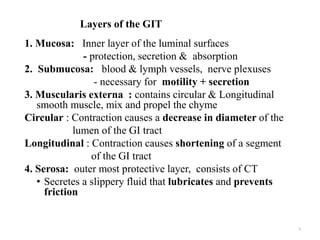
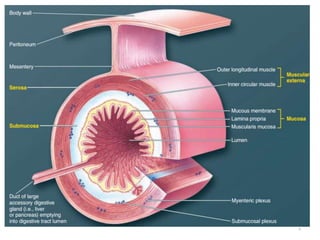
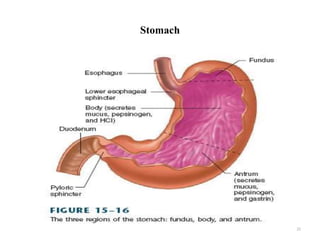
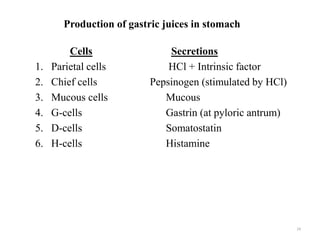
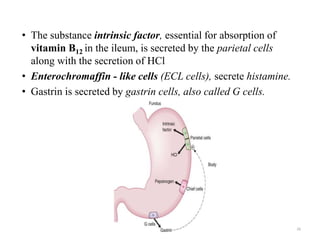
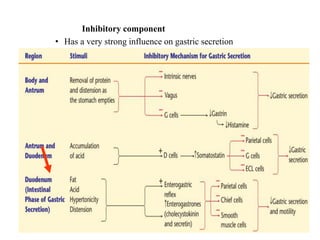
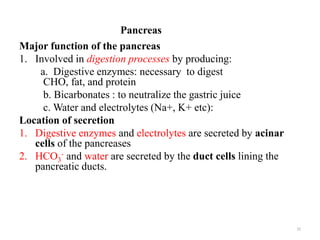
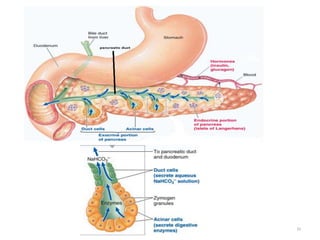
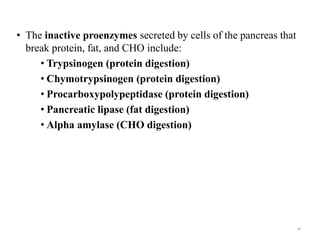
The document summarizes key aspects of gastrointestinal physiology. It describes the components and functions of the digestive system, including the layers of the gastrointestinal tract and roles of the various organs. It then discusses motility and movement of contents through the tract, the processes of mechanical and chemical digestion, and secretions and functions of saliva, stomach acid, enzymes and other factors. Motility is controlled by the enteric and autonomic nervous systems in response to stretch and chemical receptors.
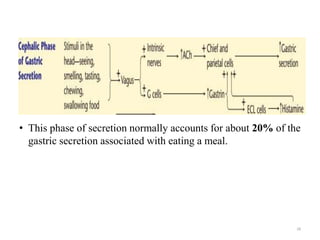
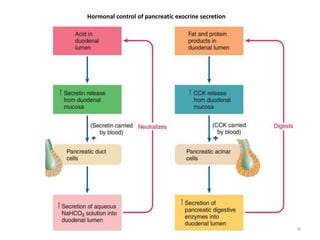
![• Cephalic phase: approximately 20% of pancreatic secretory
response to a meal
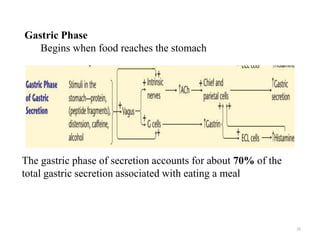
• Gastric phase: 5 to 10% of pancreatic secretory response to a
meal
Intestinal phase
• Most pancreatic secretion takes place
• Secretin(intestinal hormone) stimulates release of a large
volume of pancreatic juice with a high [HCO3-]
• Secretin is released in response to acidic chyme in the
duodenum (maximal release at pH ~ 3.0)
40](https://image.slidesharecdn.com/achapter10-git-1-220728113734-f9db2625/85/A-Chapter-10-GIT-1-pptx-40-320.jpg)