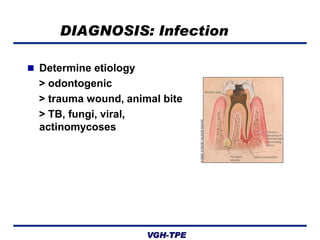
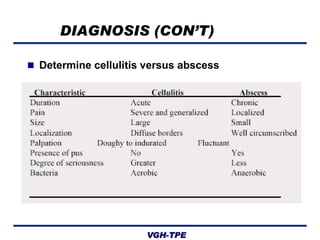
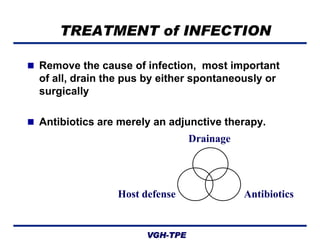
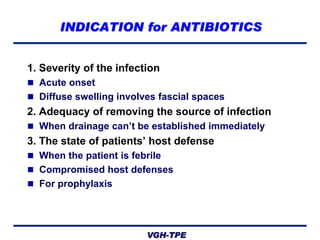
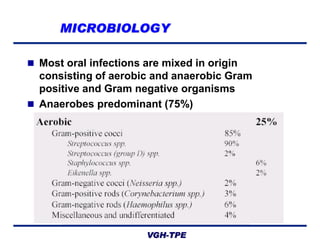
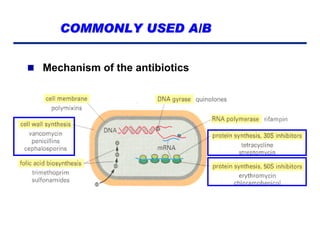
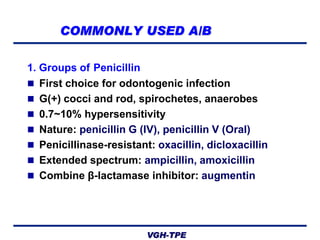
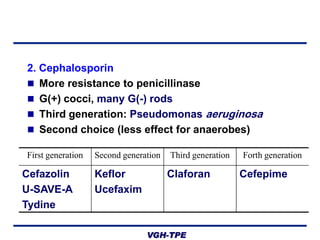
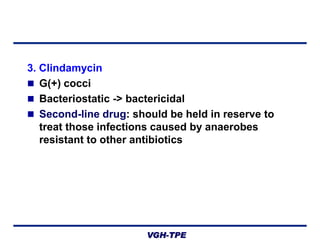
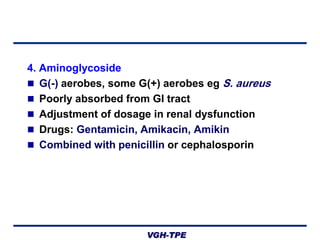
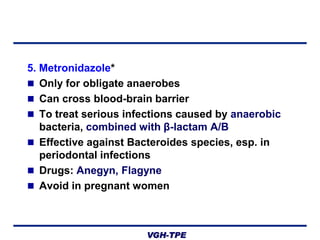
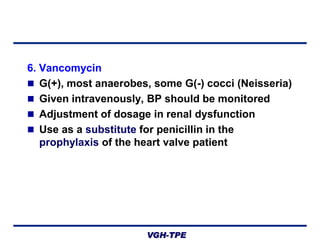
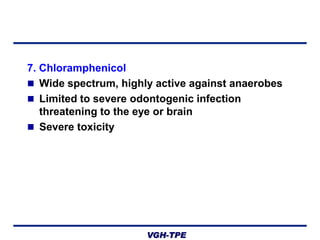
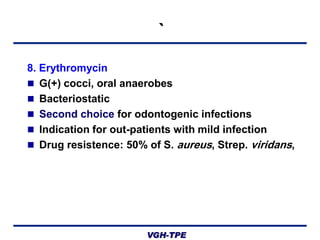
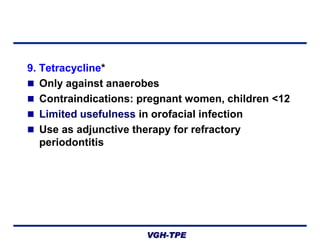
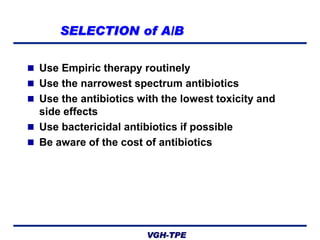
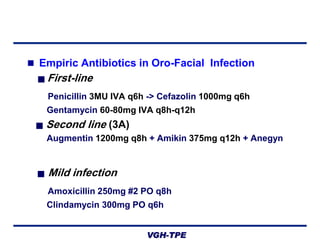
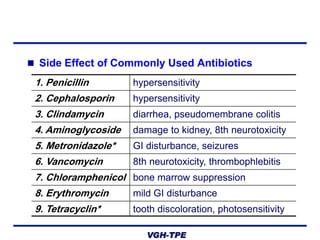
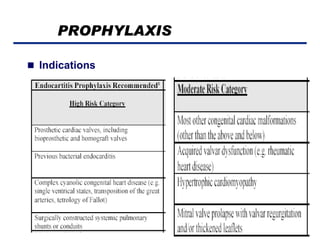
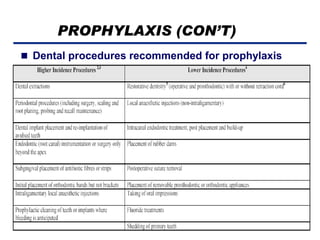
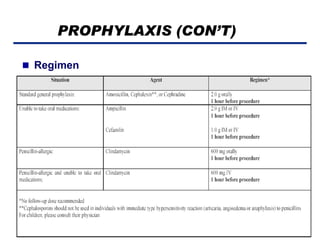
This document discusses the evaluation, diagnosis, and treatment of orofacial infections with an emphasis on antibiotic therapy and prophylaxis. It outlines how to assess infections through medical history, exam, and identifying signs of infection. Most oral infections involve both aerobic and anaerobic bacteria. Commonly used antibiotics include penicillin, cephalosporins, metronidazole, and clindamycin. Antibiotics should be used as an adjunct to drainage and are indicated for severe infections, inadequate drainage, or compromised hosts. Prophylactic antibiotics are recommended for high-risk dental procedures in certain patients.