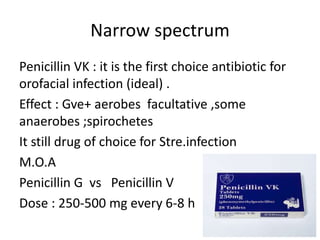
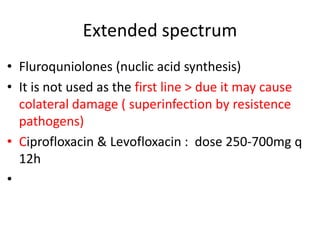
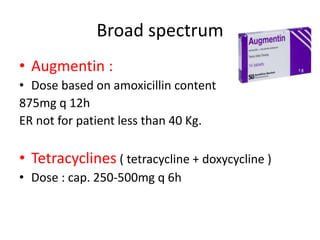
This document provides information on prescribing antibiotics for orofacial bacterial infections. It discusses appropriate antibiotic choices based on the infection type, pathogen involved, and patient factors like immunity status. Narrow-spectrum penicillins are generally first-line. It also covers prophylactic antibiotic guidelines for invasive dental procedures in high-risk cardiac and joint implant patients.