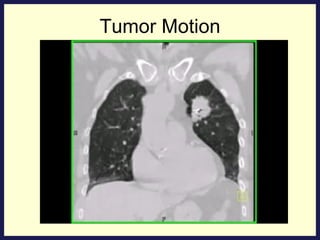
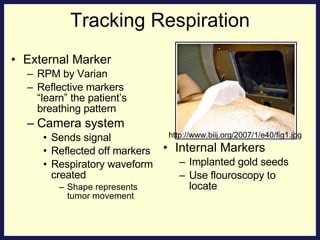
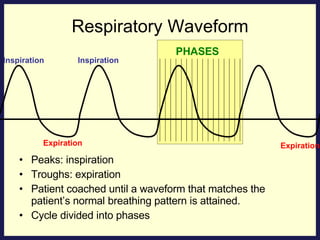
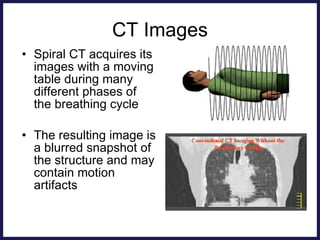
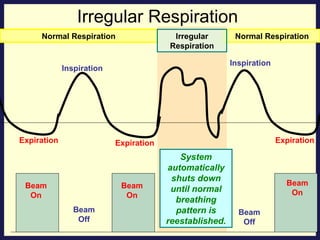
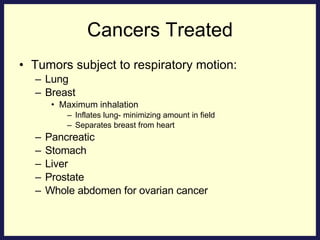
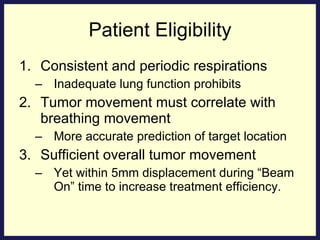
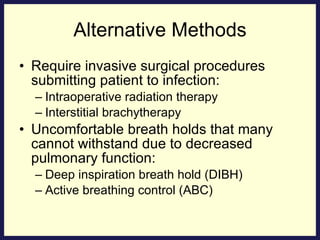
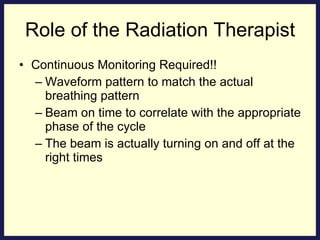
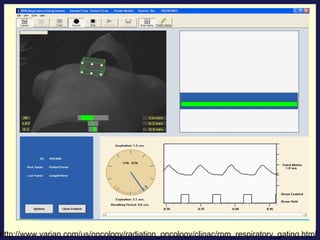
Respiratory gating with intensity-modulated radiation therapy (IMRT) allows for higher doses to be delivered to the tumor target while reducing side effects to normal tissues. It works by synchronizing beam delivery to specific phases of the respiratory cycle using external markers or internal fiducials implanted in or near the tumor. This leads to smaller planning target volumes and sharper dose gradients compared to conventional radiation therapy that does not account for tumor motion. Respiratory gating requires consistent breathing patterns from patients and continuous monitoring during treatment. It is effective for tumors in organs that move significantly during respiration like lung, liver and pancreas.