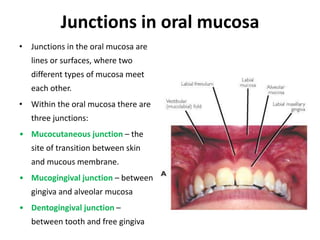
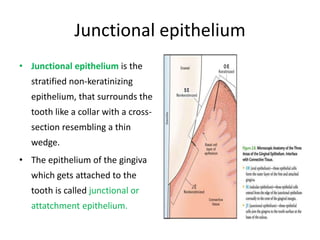
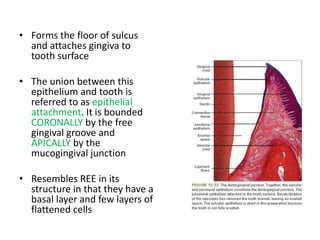
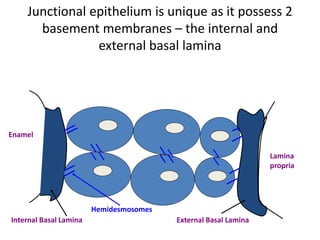
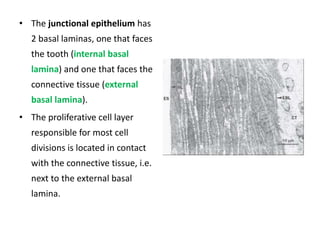
This document discusses the junctional epithelium, which is the stratified non-keratinizing epithelium that surrounds the tooth like a collar. It forms the floor of the gingival sulcus and attaches the gingiva to the tooth surface. The junctional epithelium has two basal lamina layers and is unique in that it attaches to the tooth through hemidesmosomes. It develops from the reduced enamel epithelium during tooth eruption. The junctional epithelium provides both an attachment role and a protective role through its permeability. The position of the dentogingival junction can shift through passive eruption as the gingiva recedes over time.