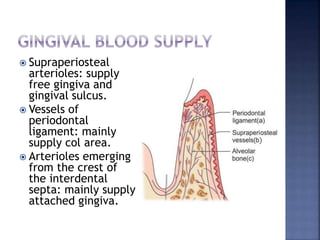
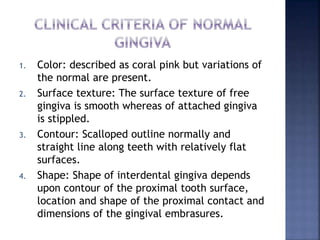
The document describes the anatomy and histology of the gingiva. It discusses that the gingiva is divided into free gingiva, interdental gingiva, and attached gingiva. It describes the epithelial layers, basement membrane, gingival fibers, blood supply, and characteristics of normal gingiva such as color, texture, contour, shape, size, and consistency.