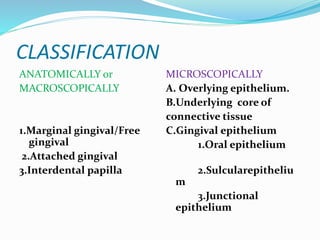
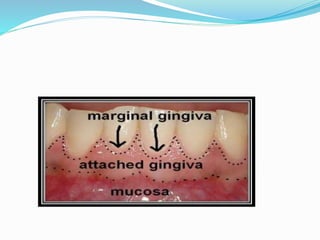
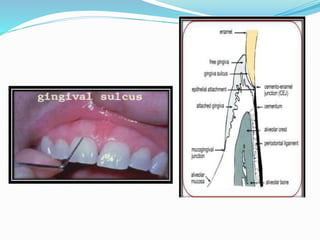
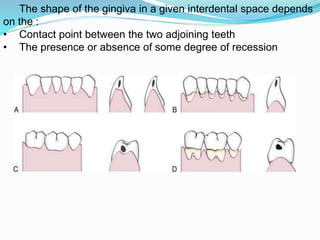
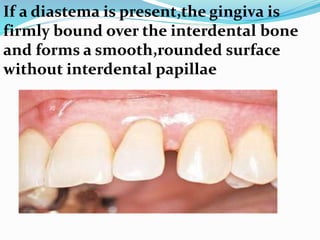
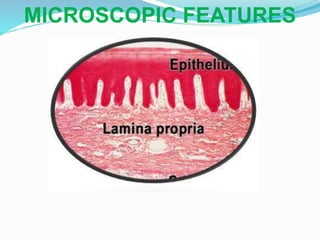
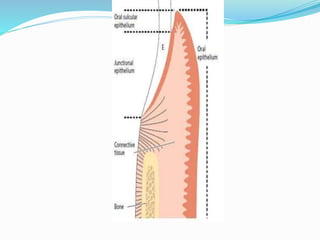
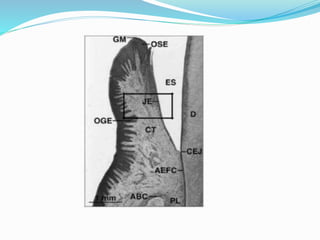
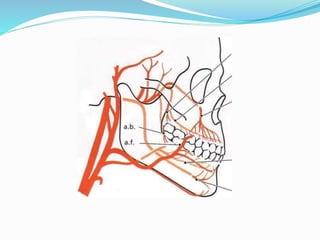
The gingiva is the gum tissue that surrounds the teeth. It has several parts - the marginal gingiva forms the border around the teeth, the attached gingiva is firmly bound to the underlying bone, and the interdental papilla fills the spaces between teeth. Microscopically, it is made of stratified squamous epithelium overlying connective tissue. The junctional epithelium attaches it to the tooth surface. The gingiva provides protection and resilience to withstand forces from chewing. With age, it thins but dental plaque buildup can lead to gingivitis and periodontal disease if not removed.