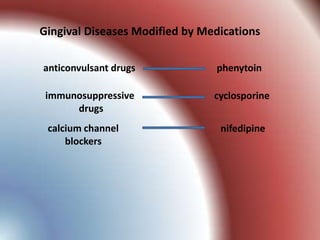
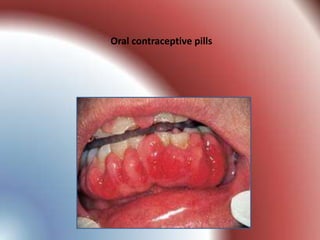
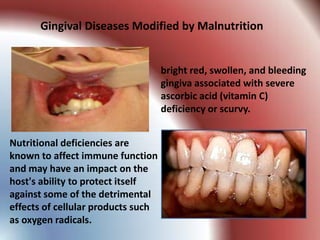
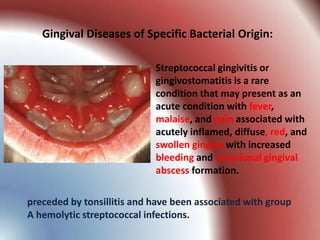
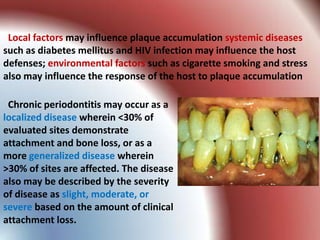
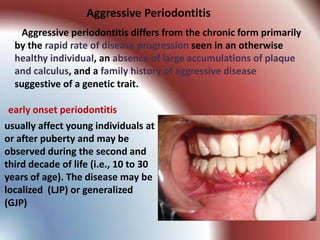
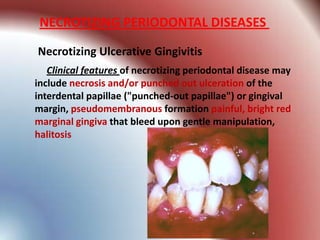
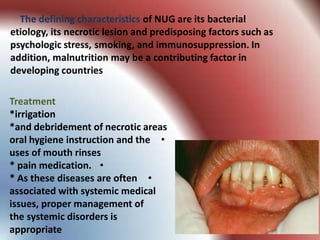
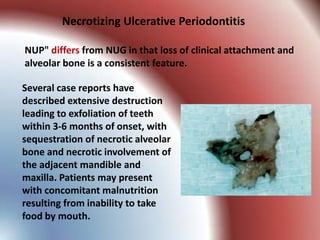
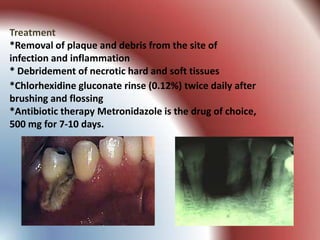
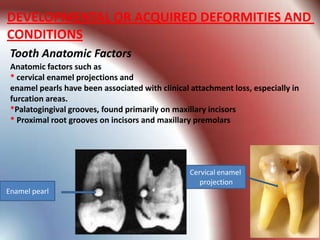
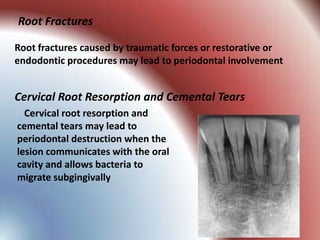
This document summarizes various gingival and periodontal diseases. It describes diseases caused by dental plaque, such as gingivitis, and modified by factors like medications, malnutrition, and systemic diseases. It also discusses periodontitis and other conditions like necrotizing gingivitis/periodontitis, endo-perio lesions, and developmental deformities that can affect the gingiva and periodontium. Diagnostic methods and typical treatments are mentioned for several conditions.