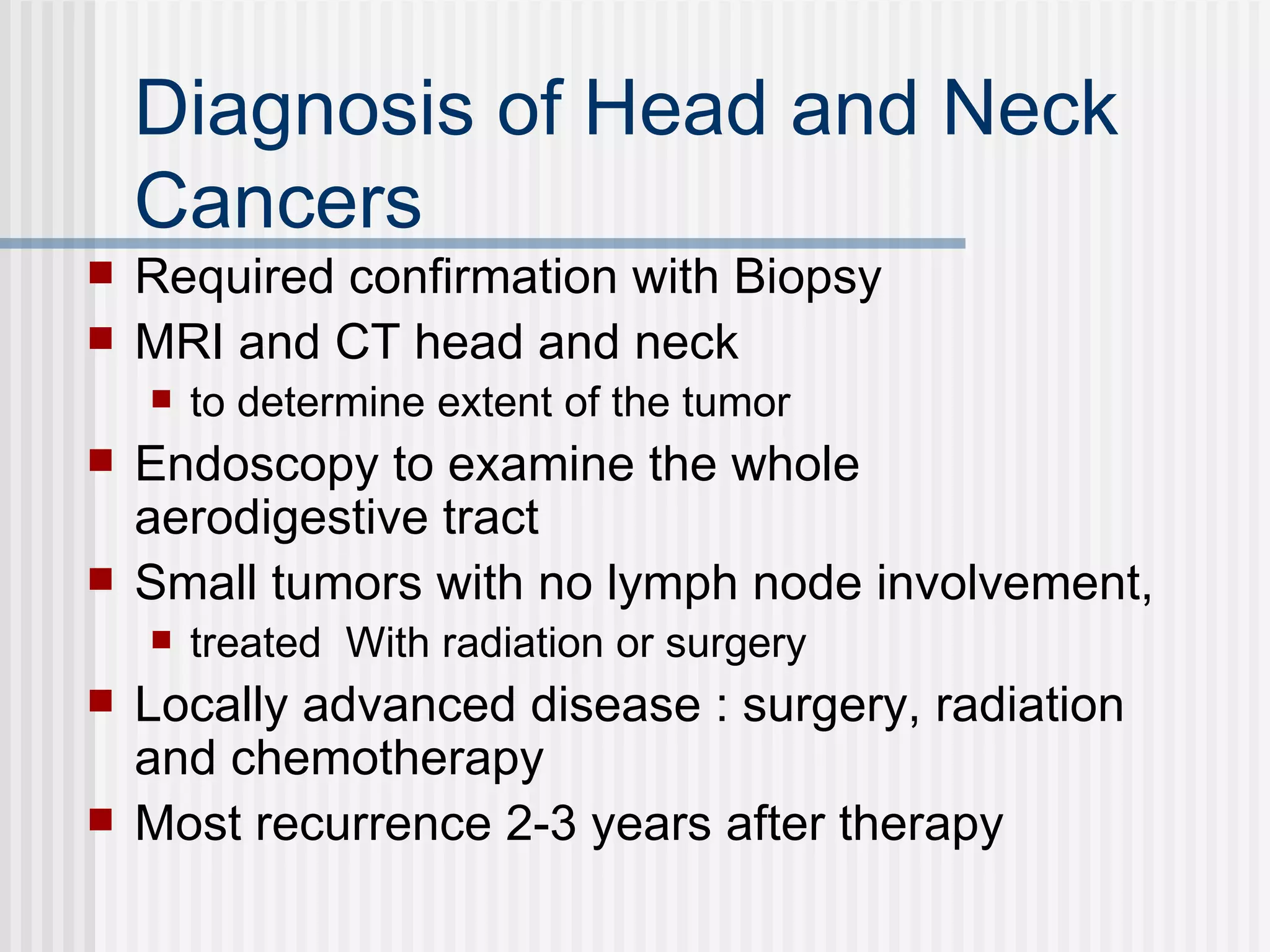
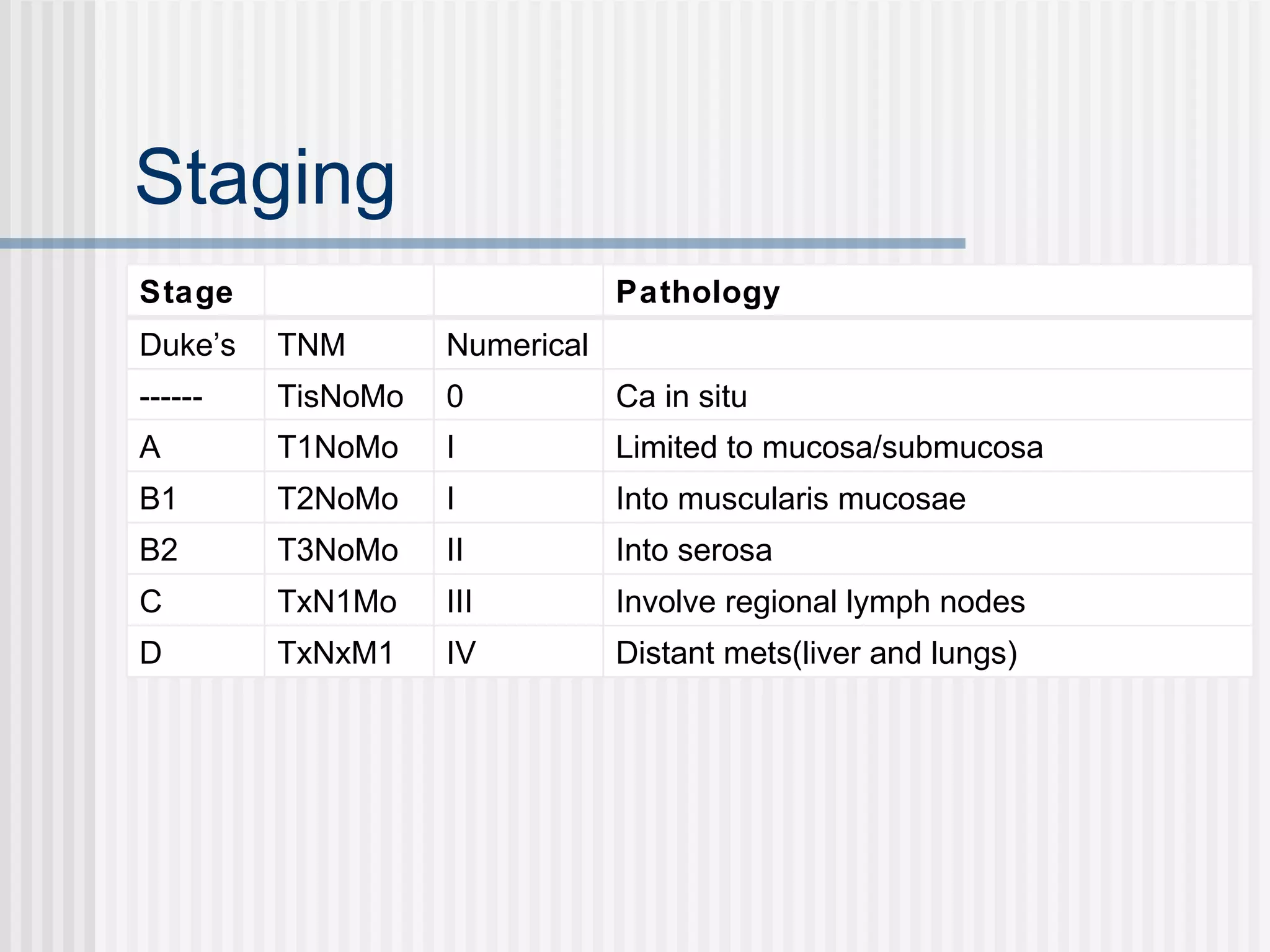
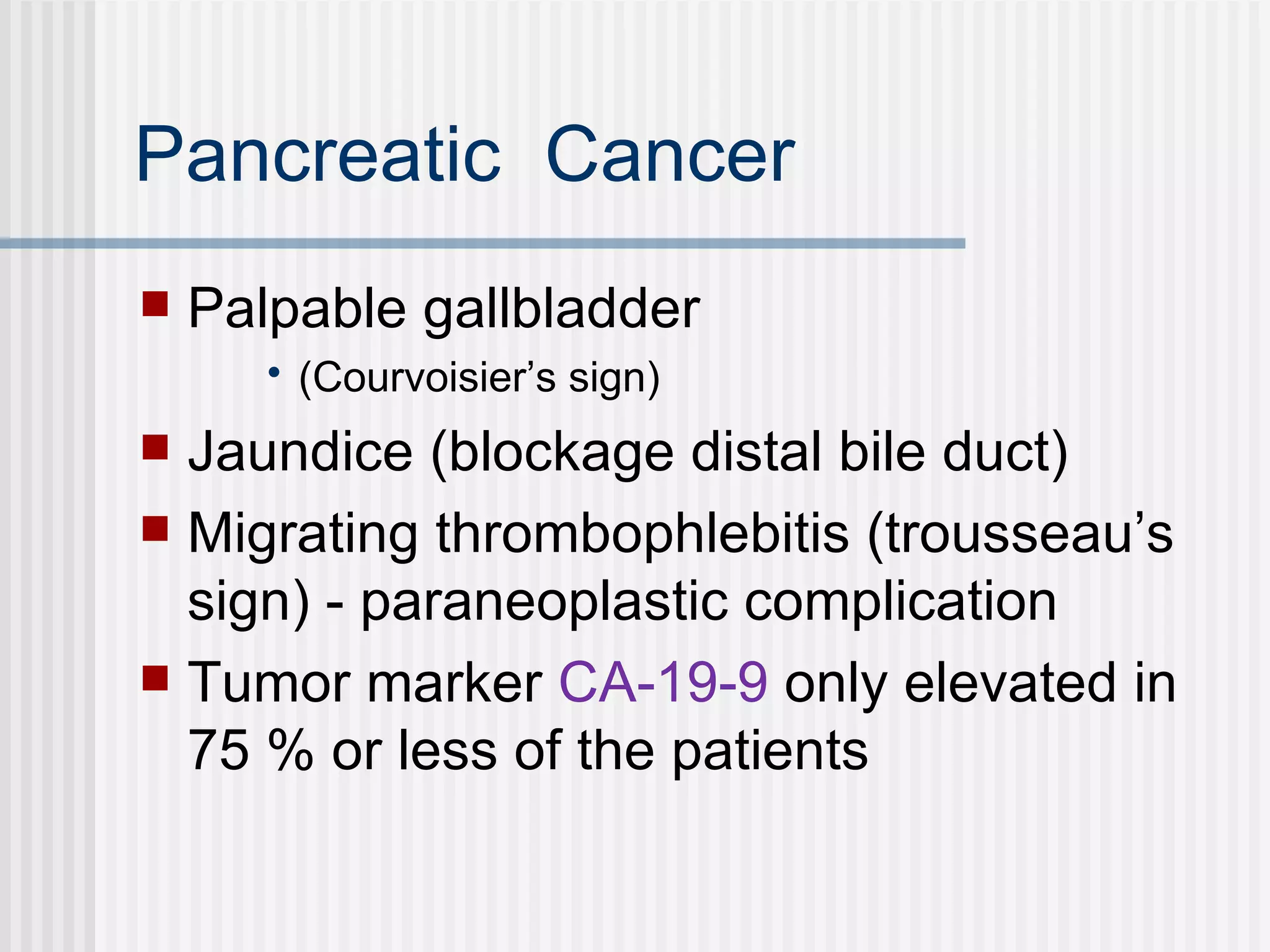
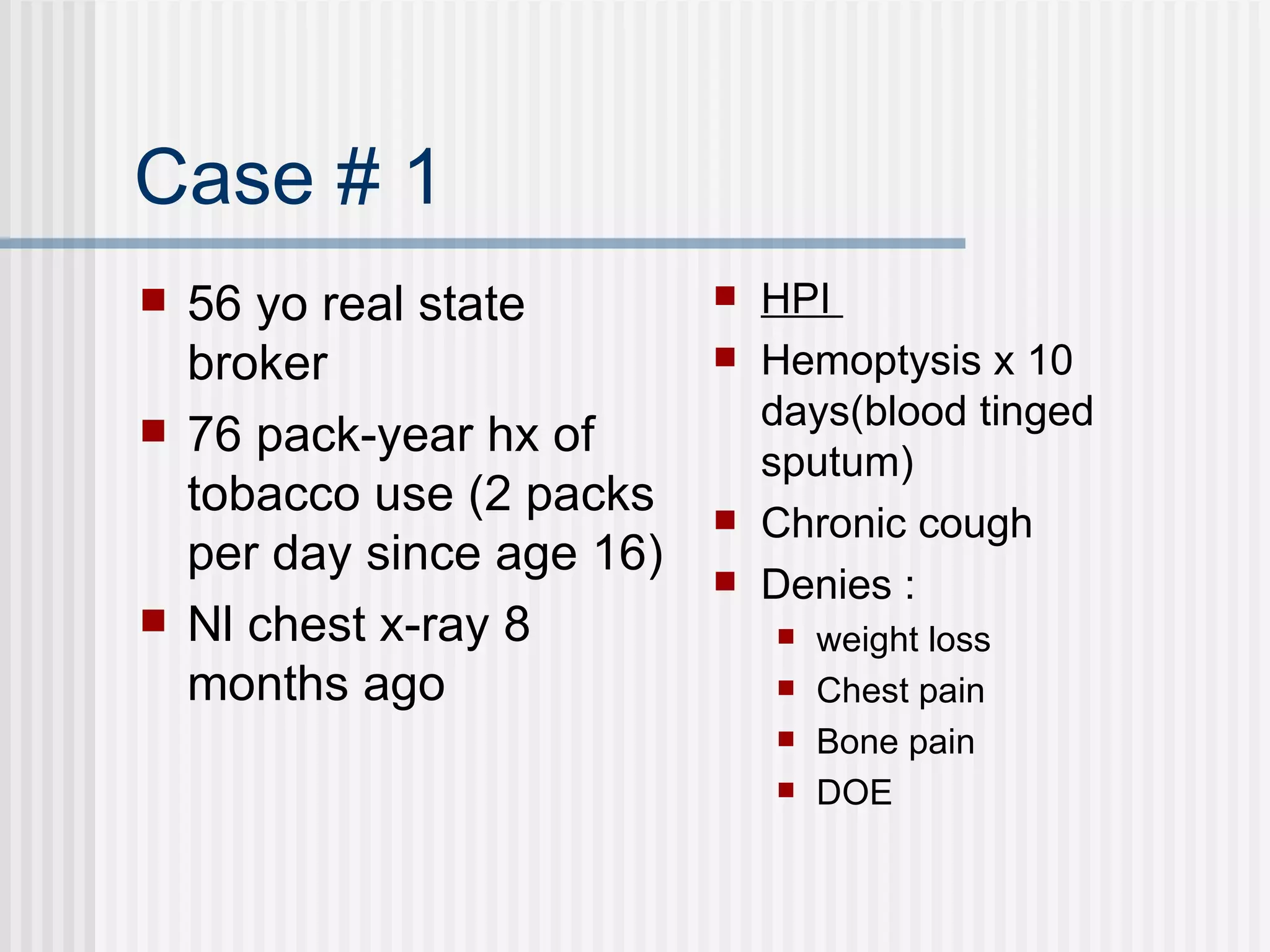
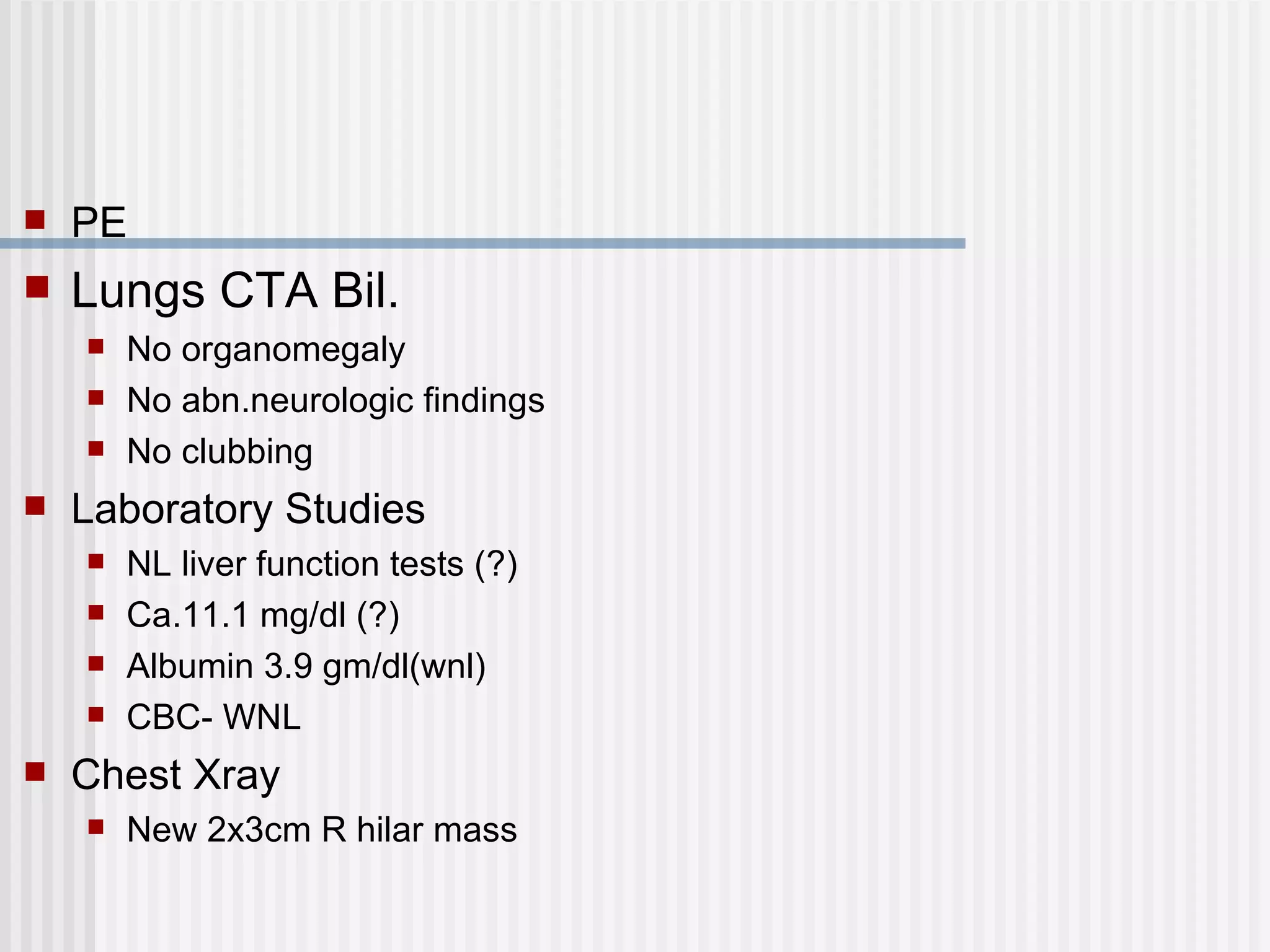
This document summarizes information about several types of solid tumors. It provides details about a 56 year old male patient presenting with hemoptysis and a lung mass. It discusses risk factors, symptoms, diagnostic tests and staging for lung cancer. It also summarizes information about other cancers such as head and neck, esophageal, gastric, colorectal, pancreatic and anal cancers.

![Smoking There are more than 60 molecules in cigarette smoke that are thought to be carcinogenic in humans Two carcinogens highly associated with lung cancer are benzo[a]pyrene and N-nitrosamine NNK. These molecules bind to DNA and proteins , forming adducts . The presence of adducts increases the chance of DNA mutation and interferes with the proper function of proteins](https://image.slidesharecdn.com/2solidtumors1-090304135624-phpapp01/75/2-Solid-Tumors1-15-2048.jpg)