This document presents two case studies.
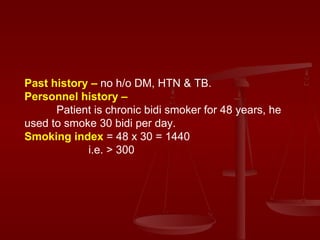
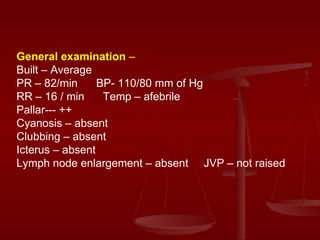
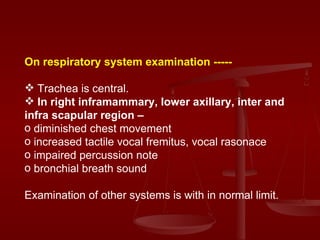
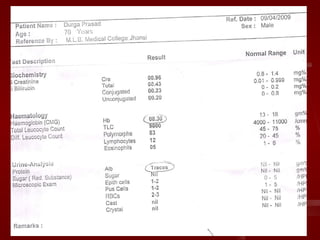
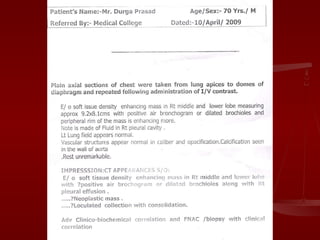
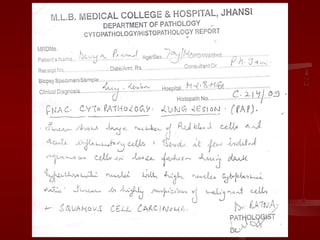
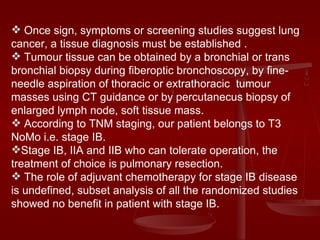
Case 1 is a 70-year-old male farmer with an 8-month history of cough, appetite loss, and weight loss. Examination found diminished breath sounds in the right lung. Imaging and biopsy revealed squamous cell carcinoma involving the right middle and lower lobes.
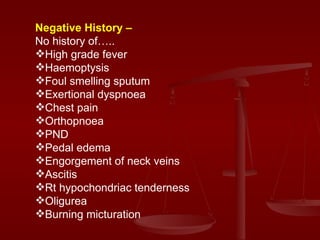
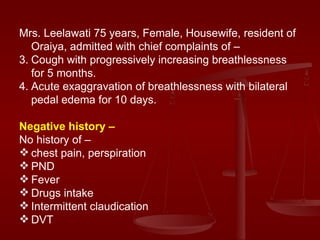
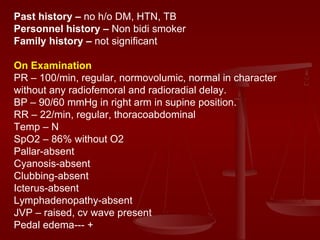
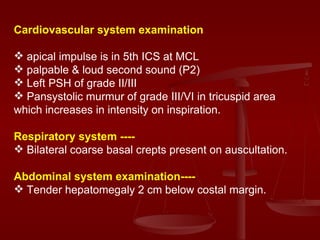
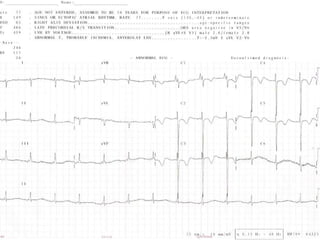
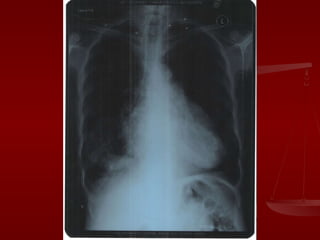
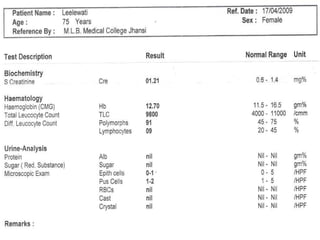
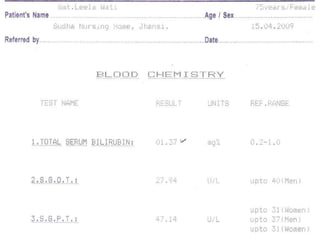
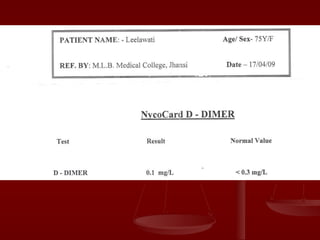
Case 2 is a 75-year-old female housewife with 5 months of cough and progressive breathlessness, exacerbated for 10 days with leg swelling. Examination found elevated jugular venous pressure, leg swelling, and heart murmur. Investigations supported a diagnosis of pulmonary hypertension due to chronic obstructive airway disease.