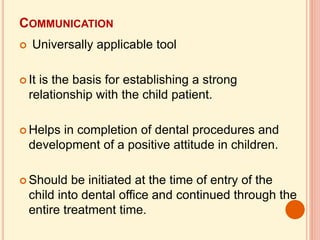
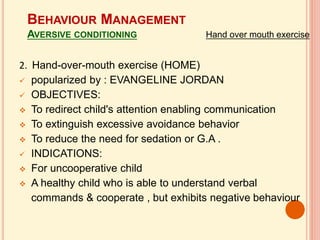
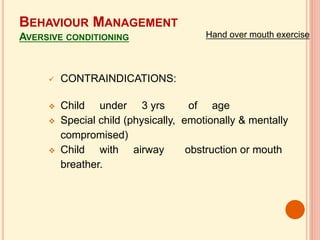
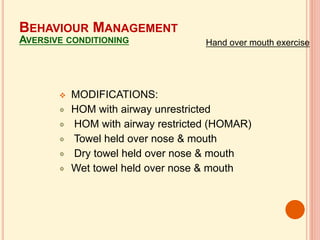
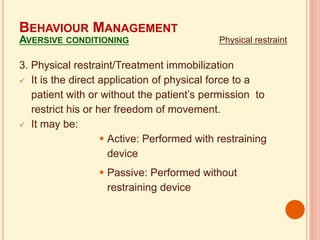
This document discusses various non-pharmacological behavior management techniques used in pediatric dentistry. It covers communication techniques, behavior modification including desensitization, modeling and contingency management. It also discusses pre-appointment preparation and techniques like voice control, hand-over-mouth exercise, physical restraint, implosion therapy, and retraining that aim to modify disruptive behaviors in children undergoing dental treatment.