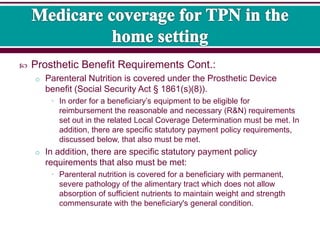
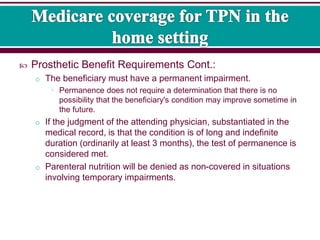
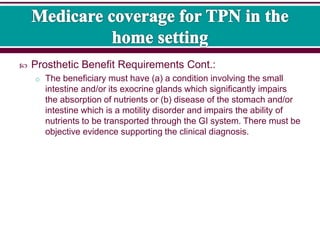
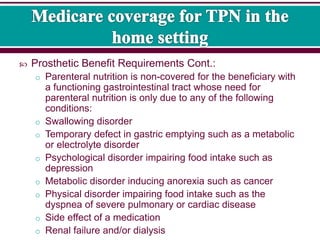
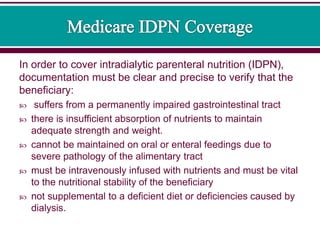
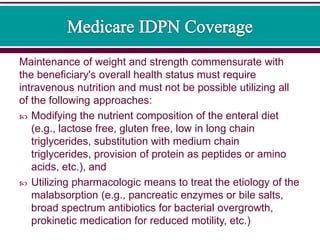
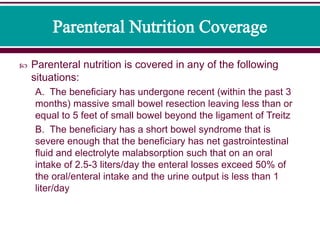
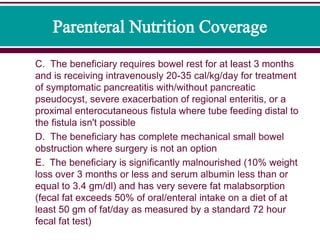
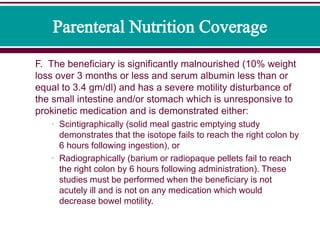
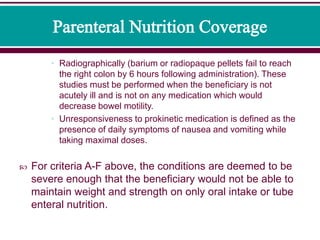
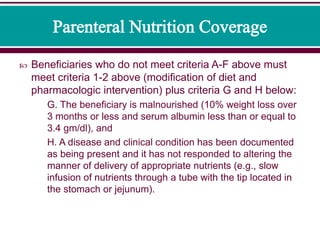
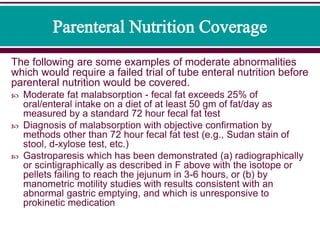
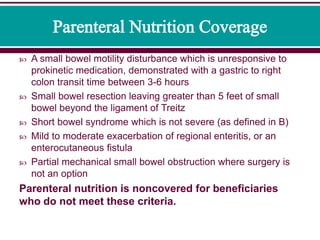
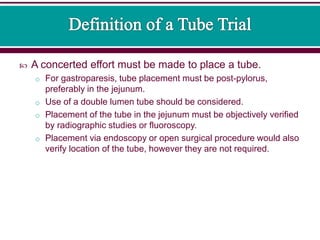
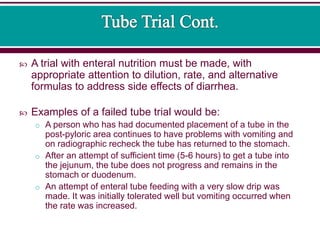
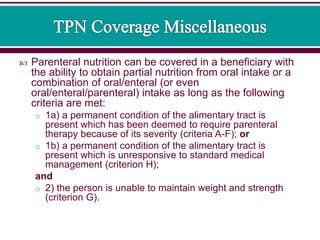
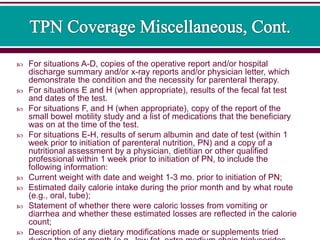
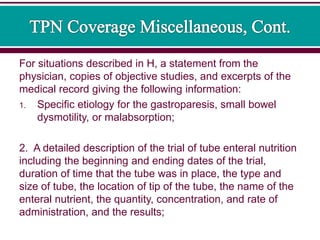
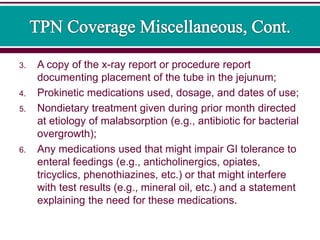
The document discusses guidelines for determining insurance coverage of home parenteral nutrition (PN). Coverage requires a permanent condition preventing sufficient oral nutrient absorption. Specific criteria include short bowel syndrome, malabsorption, or motility disorders unresponsive to other interventions. Initiation of PN requires documentation of the condition and failed enteral nutrition trials. Ongoing coverage requires monitoring that the criteria supporting medical necessity are still met.