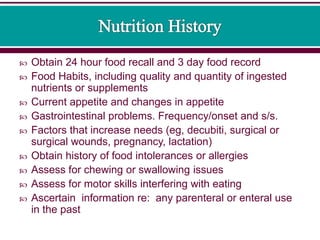
A comprehensive nutritional assessment should be performed prior to central line placement for parenteral nutrition (PN) and include anthropometrics, clinical information, nutrition intake history, and biochemical data. This assessment establishes baseline nutrition measurements, identifies deficits, determines risk factors, and identifies medical or psychosocial factors influencing nutritional support. The goals are to achieve adequate nutritional status and determine if malnutrition is present or developing. Nutritional support and monitoring must be an ongoing process. Parenteral nutrition requiring access to a central vein requires documentation of proper central line placement in the superior vena cava.