This document provides information on parenteral nutrition including:
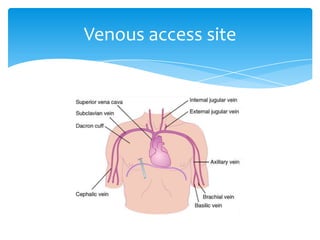
- Parenteral nutrition involves infusing complete nutrient solutions directly into the bloodstream via a central or peripheral vein to meet nutritional needs.
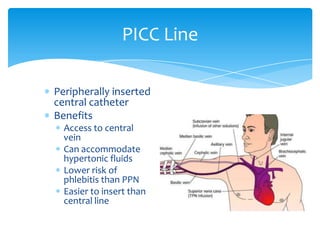
- It can be delivered through either total parenteral nutrition (TPN) using a central line, or peripheral parenteral nutrition (PPN) using a peripheral vein or peripherally inserted central catheter (PICC) line.
- PPN has limitations as the peripheral sites are more prone to inflammation/infection and the catheter may need repeated insertion, while TPN is preferred for long-term nutrition support.
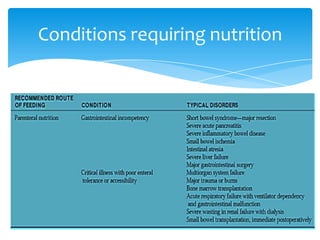
- Indications for parenteral nutrition include when the gastrointestinal tract is non-functioning or unable to meet