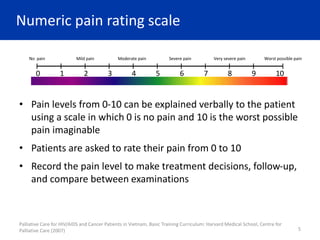
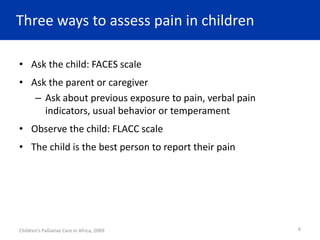
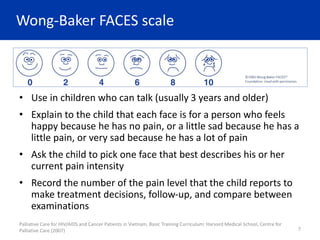
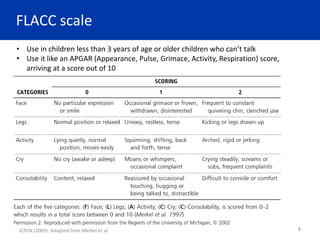
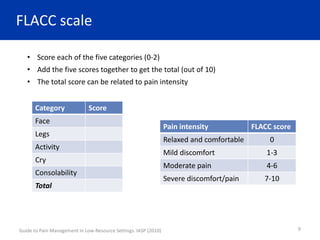
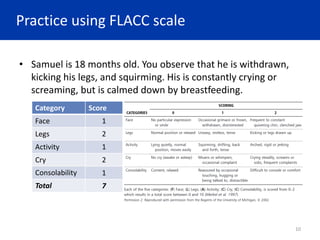
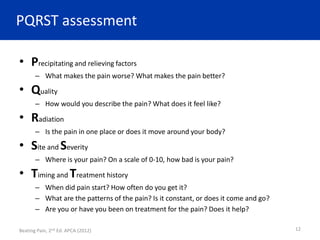
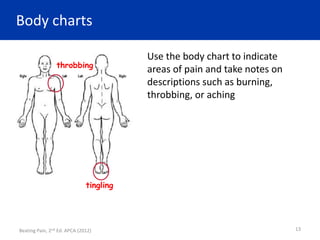
This document discusses pain assessment tools including scales to measure pain. It describes the numeric pain rating scale from 0-10, the Wong-Baker FACES scale for children who can communicate, and the FLACC scale to assess pain in children who cannot communicate verbally. The FLACC scale evaluates five categories: face, legs, activity, cry, and consolability. Scores are summed to assess overall pain intensity. Detailed pain assessments using tools like the PQRST method and body charts can provide more information on pain location, type, and response to treatment. Accurately measuring pain using validated scales helps ensure appropriate pain management for patients.
![References
• African Palliative Care Association. Beating Pain: a pocketguide for pain
management in Africa, 2nd Ed. [Internet]. 2012. Available from:
http://www.africanpalliativecare.org/images/stories/pdf/beating_pain.pdf
• African Palliative Care Association. Using opioids to manage pain: a pocket guide
for health professionals in Africa [Internet]. 2010. Available from:
http://www.africanpalliativecare.org/images/stories/pdf/using_opiods.pdf
• Amery J, editor. Children’s Palliative Care in Africa [Internet]. 2009. Available from:
http://www.icpcn.org/wp-content/uploads/2013/08/Childrens-Palliative-Care-in-
Africa-Full-Text.pdf
• Kopf A, Patel N, editors. Guide to Pain Management in Low-Resource Settings
[Internet]. 2010. Available from: http://www.iasp-
pain.org/files/Content/ContentFolders/Publications2/FreeBooks/Guide_to_Pain_
Management_in_Low-Resource_Settings.pdf
• The Palliative Care Association of Uganda and the Uganda Ministry of Health.
Introductory Palliative Care Course for Healthcare Professionals. 2013.
15](https://image.slidesharecdn.com/3-230607155025-454ccb1f/85/3-Pain-Assessment-pptx-15-320.jpg)