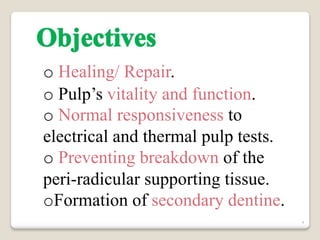
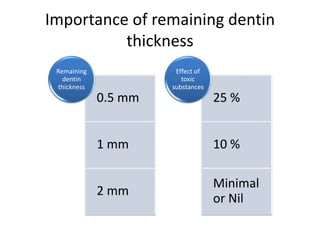
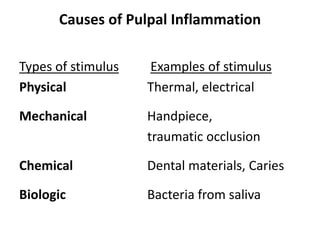
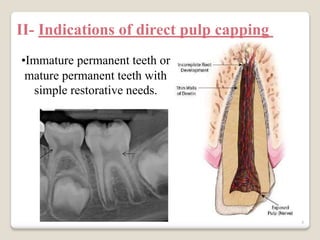
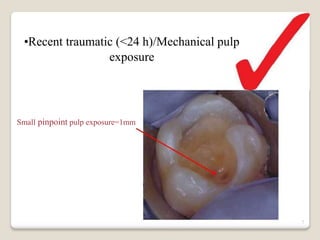
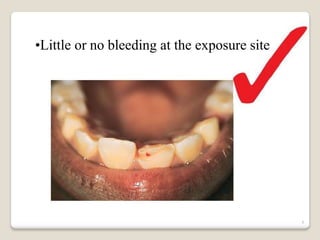
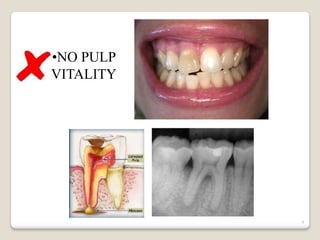
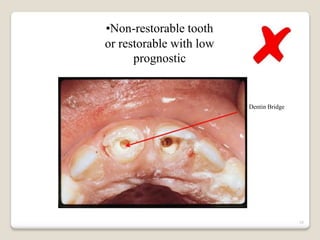
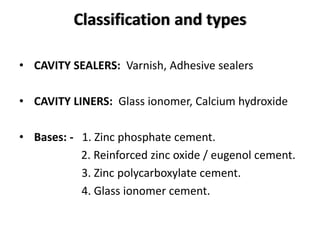
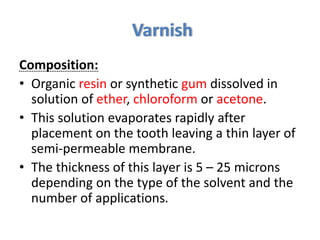
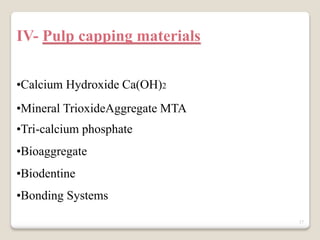
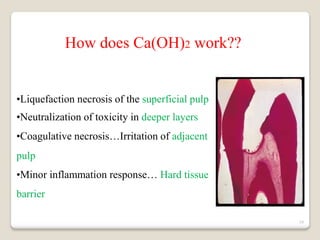
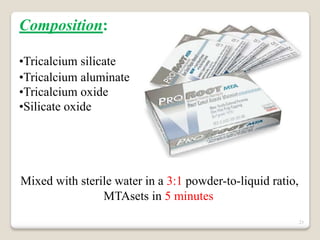
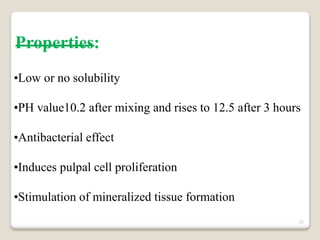
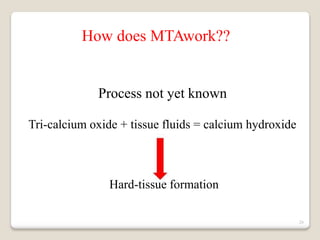
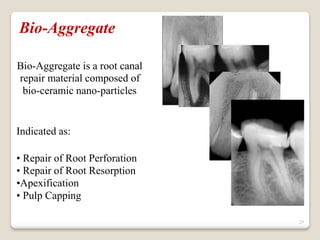
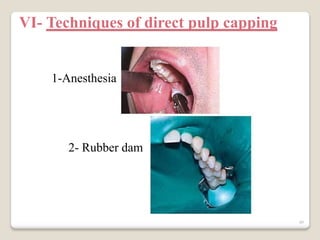
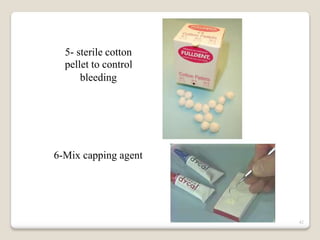
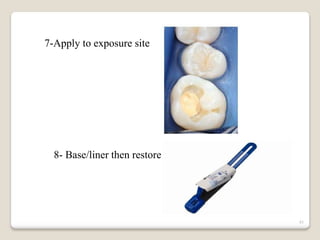
This document discusses various aspects of direct pulp capping procedures including indications, materials, and techniques. It provides information on different types of pulp capping materials like calcium hydroxide, MTA, Biodentine and their properties and mechanisms of action in pulp healing and dentin bridge formation. The document also outlines the steps of direct pulp capping techniques including isolation, controlling bleeding, application of the capping material and restoration. Bases are described as providing insulation, bulk build up and blocking of undercuts under restorations.