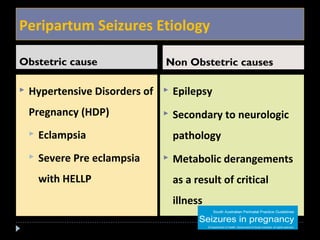
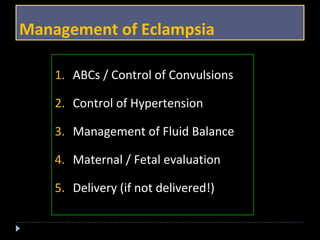
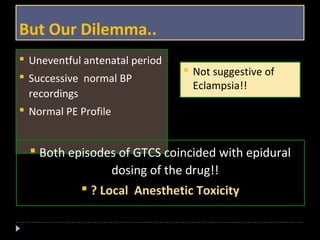
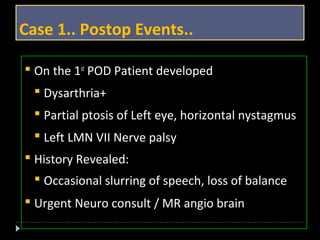
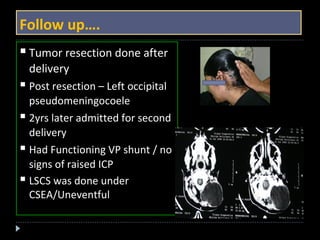
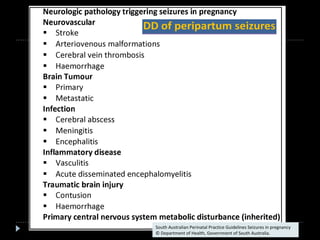
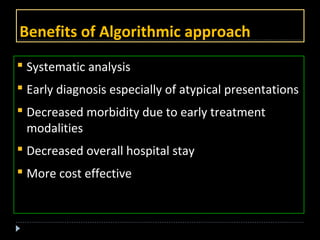
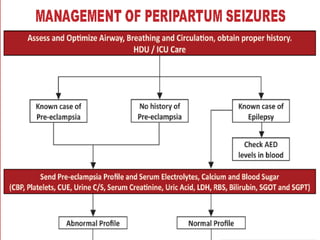
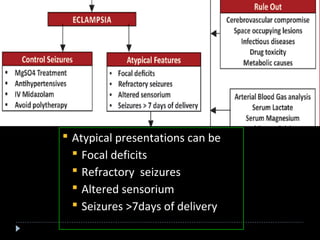
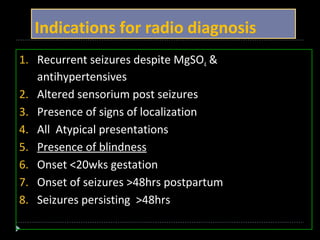
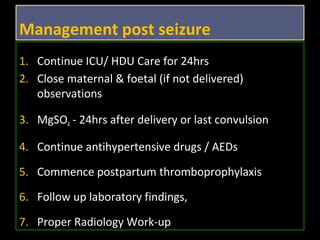
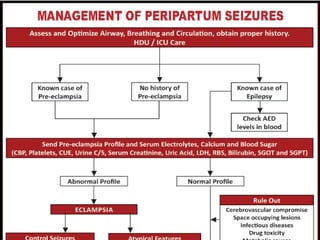
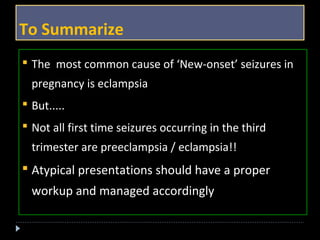
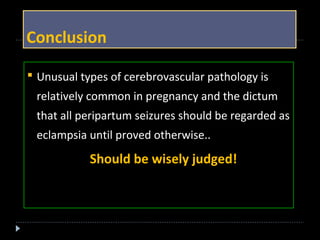
This document discusses peripartum seizures and provides several case studies. It outlines an algorithmic approach for evaluating and managing peripartum seizures. Causes can include preeclampsia, eclampsia, epilepsy, or other neurological conditions. Initial treatment involves magnesium sulfate, controlling blood pressure and monitoring. Atypical presentations require further investigation like imaging to rule out conditions like cerebral venous sinus thrombosis. MRI is generally preferred over CT for imaging during pregnancy due to risks of radiation and better detection of conditions like posterior reversible encephalopathy syndrome. Management after delivery includes continued magnesium sulfate, antihypertensives, anticonvulsants and thromboprophylaxis as needed.