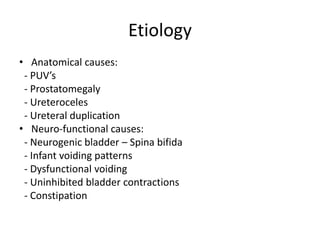
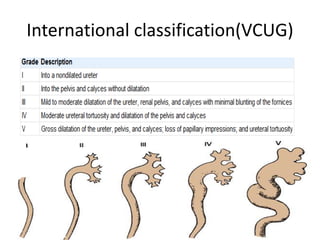
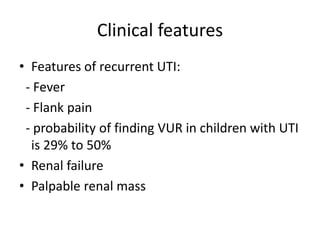
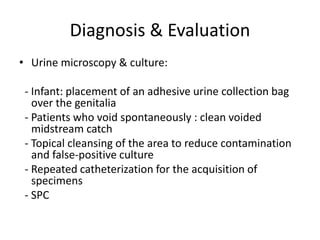
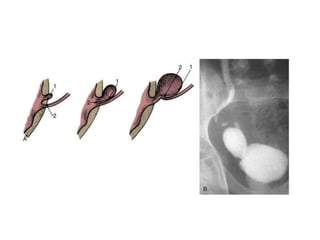
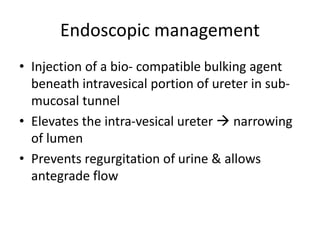
Vesicoureteral reflux (VUR) is retrograde flow of urine from the bladder to the upper urinary tract. It can be primary due to deficiencies in the ureterovesical junction or secondary due to bladder dysfunction. Diagnosis involves urine tests, ultrasound, VCUG, DMSA scan and urodynamic studies. Most low-grade reflux resolves spontaneously while high-grade reflux is less likely to resolve. Management includes antibiotics and watchful waiting or surgical correction via open or endoscopic techniques like injection of bulking agents. The goal is to prevent urinary tract infections and renal damage.