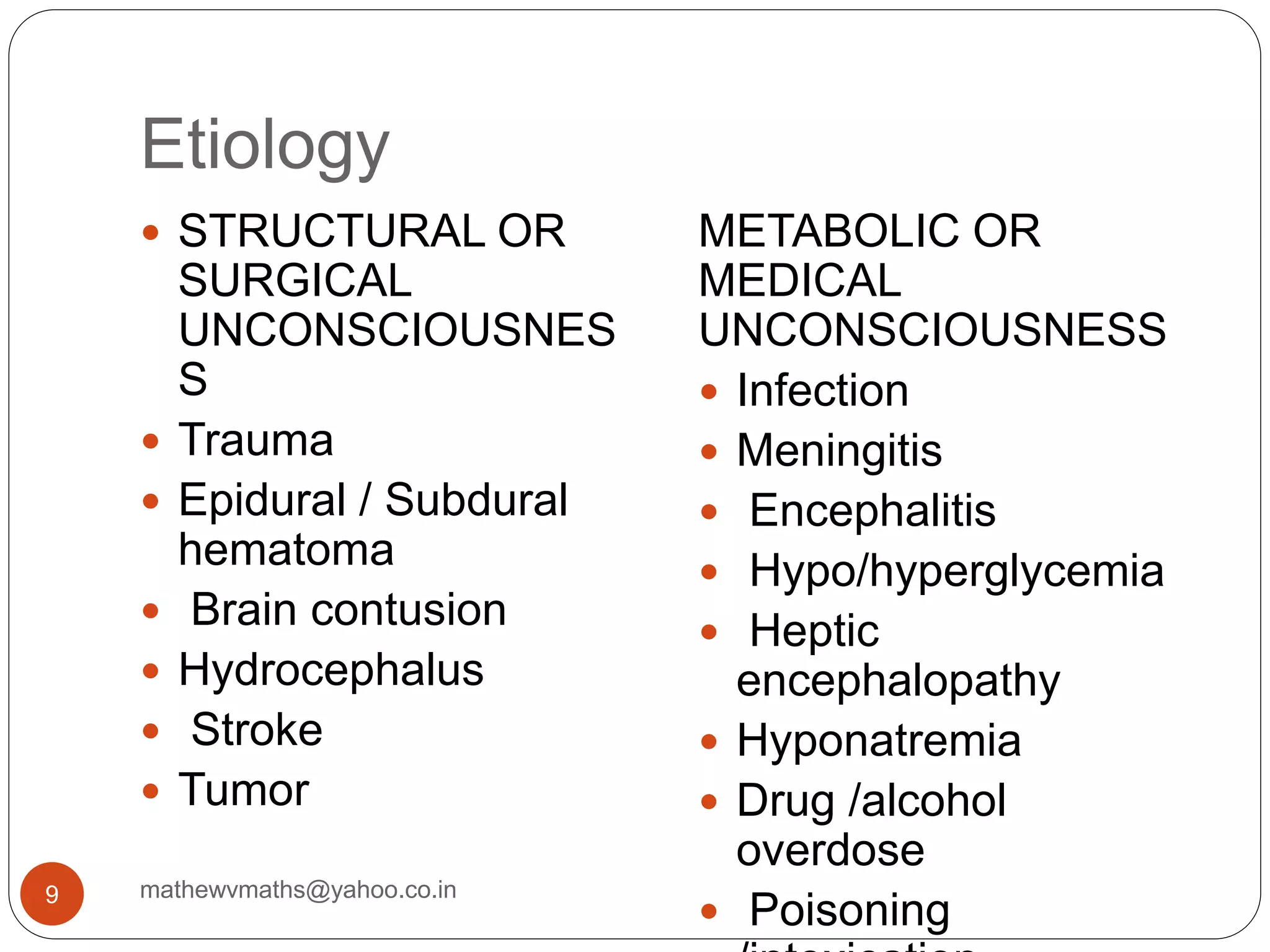
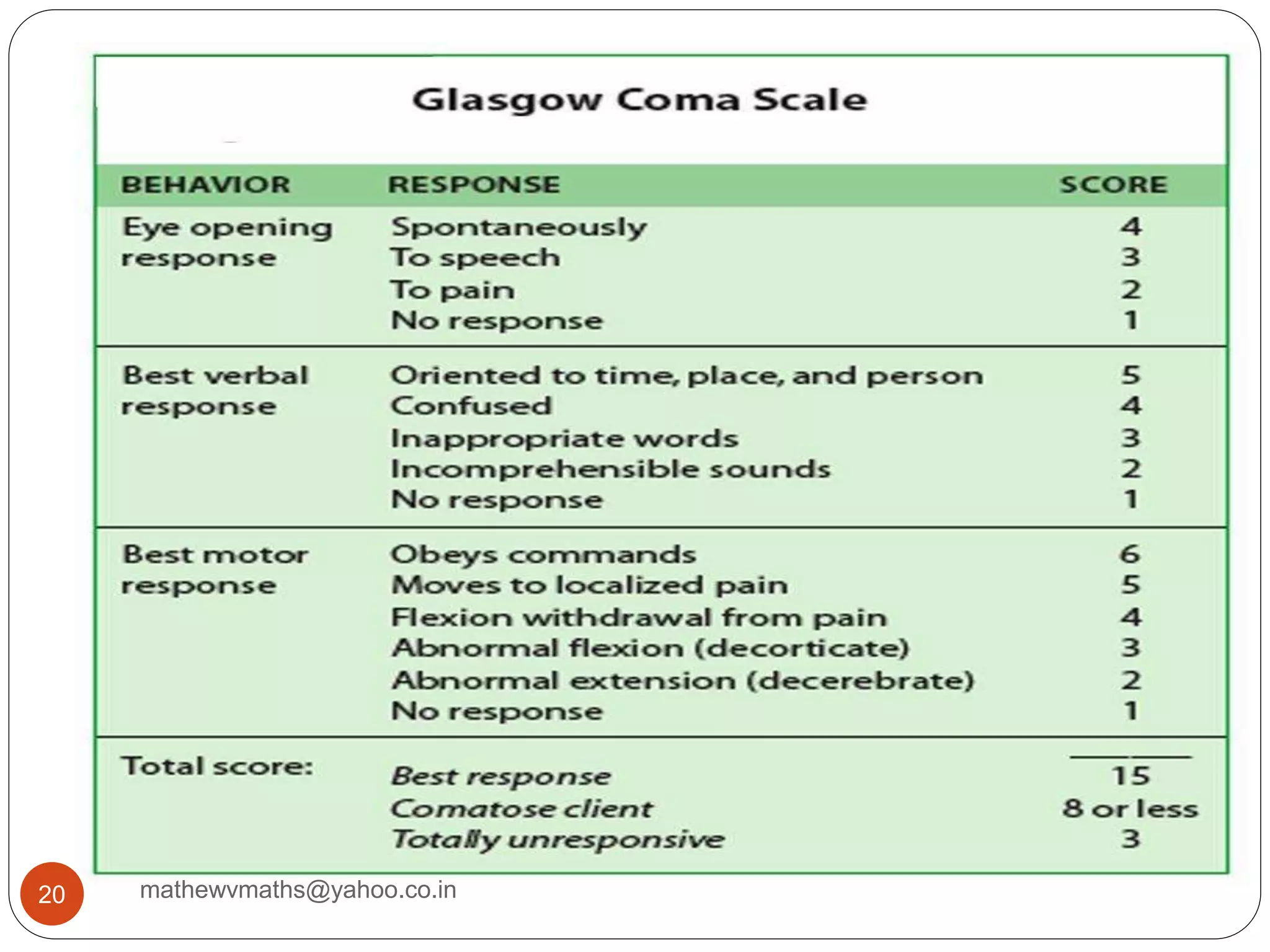
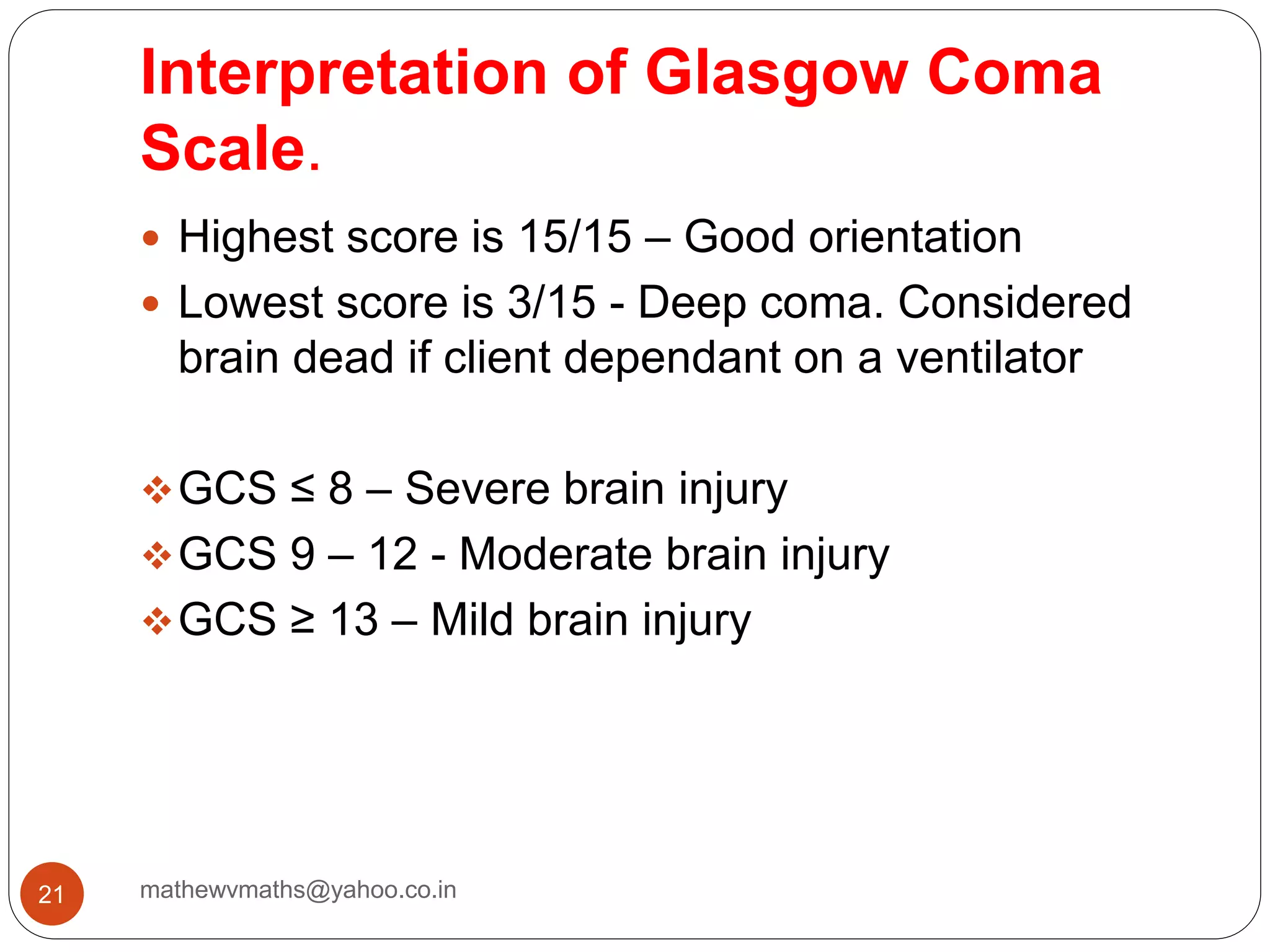
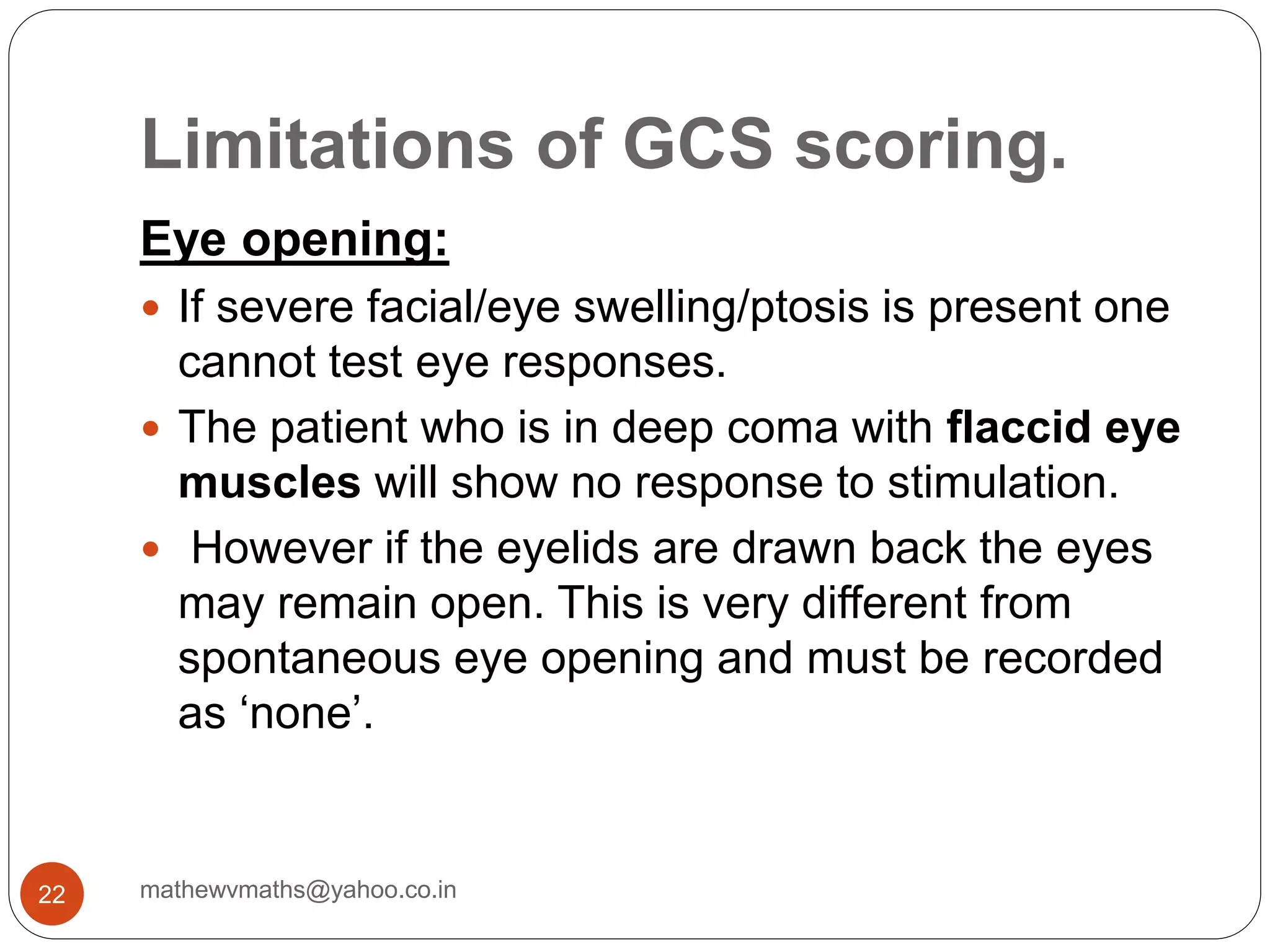
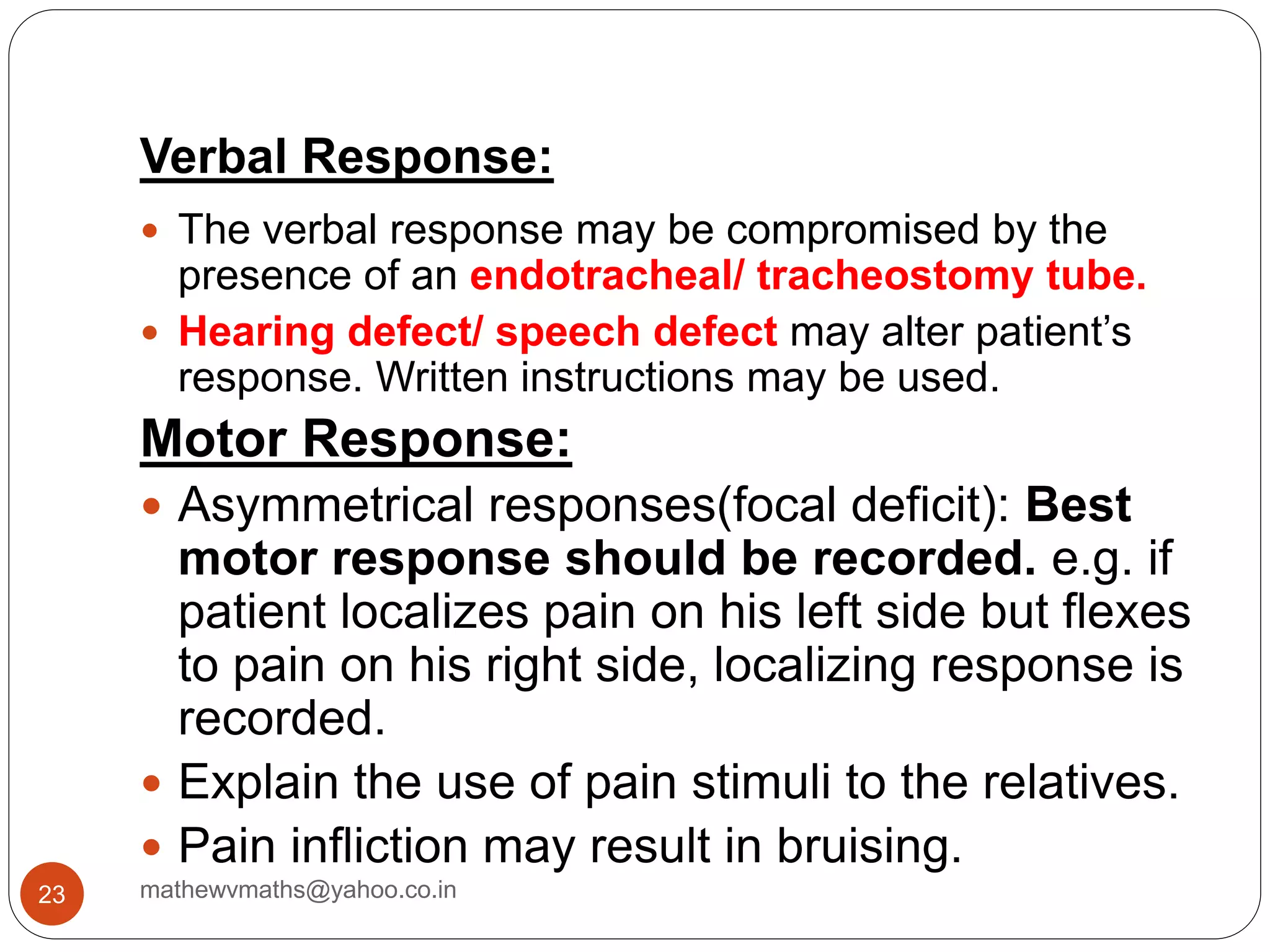
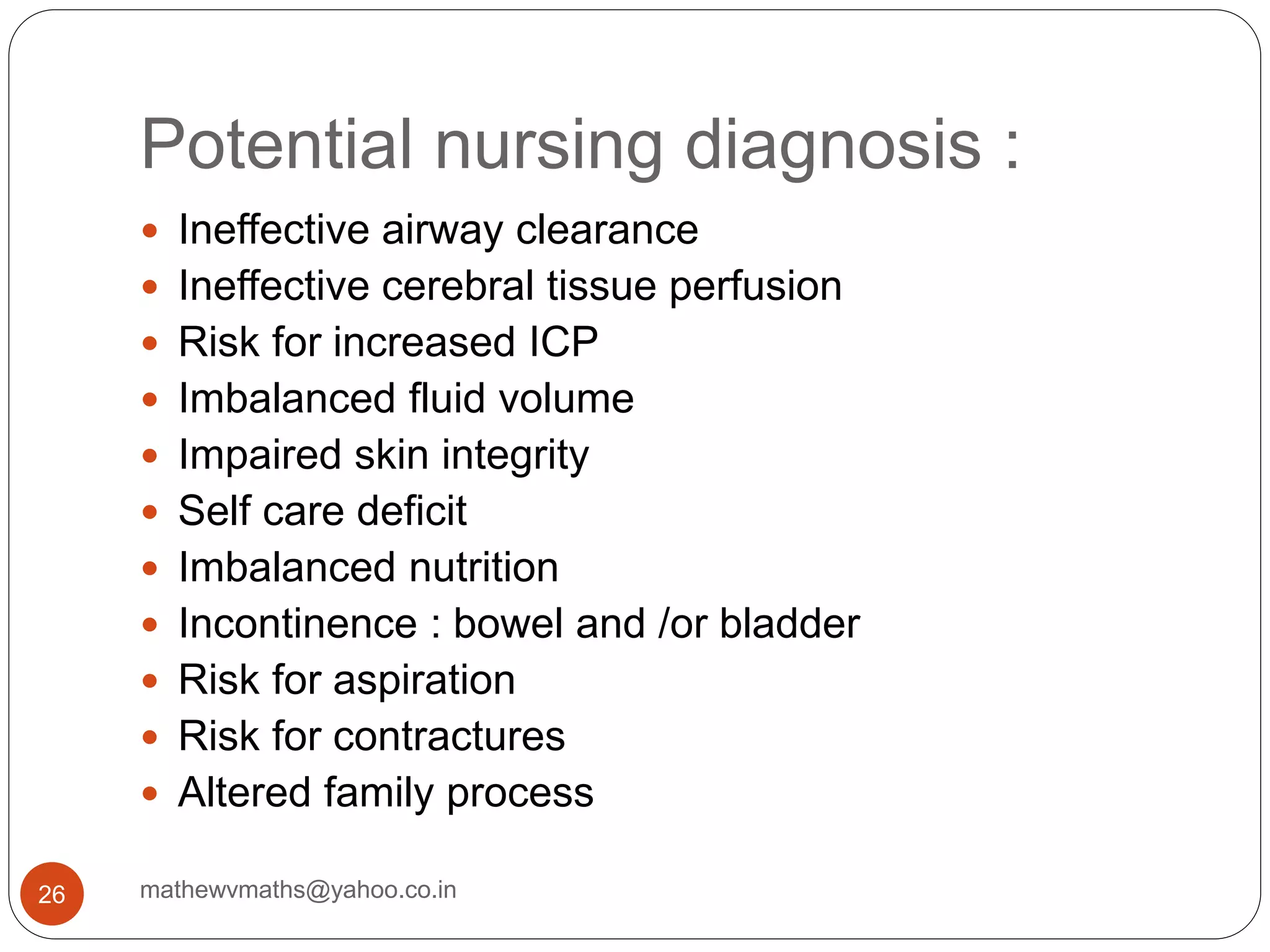
The document discusses nursing care for unconscious patients. It begins by defining unconsciousness and describing the reticular activating system's role in consciousness. Potential causes of unconsciousness include trauma, infection, drugs or alcohol. Nursing management aims to maintain adequate cerebral perfusion and function, including careful monitoring, positioning, airway care, and treatment of increased intracranial pressure if present. Assessment tools like the Glasgow Coma Scale are used to evaluate responses and guide care of the unconscious patient.


















![ Schedule care so that harsh activity [suctioning
,bathing, turning] are not grouped together, with
breaks between care for recovery.
Talk softly and limit touch and stimulation.
Administer laxatives, antitussives and antiemetics
as ordered
Manage temperature with antipyretics and cooling
measures.
Prevent seizure with ordered dilantin.
Administer mannitol 25-50 g IV bolus if ICP >20,
as prescribed.
30 mathewvmaths@yahoo.co.in](https://image.slidesharecdn.com/nursingcareofunconsc-190903145102/75/Nursing-care-of-unconscious-Patient-30-2048.jpg)