The document summarizes information about liver function tests and bilirubin metabolism. It discusses:
- Liver function tests measure enzyme and protein levels to evaluate liver health and function. They can screen for disease, determine disease patterns, and assess severity and treatment response.
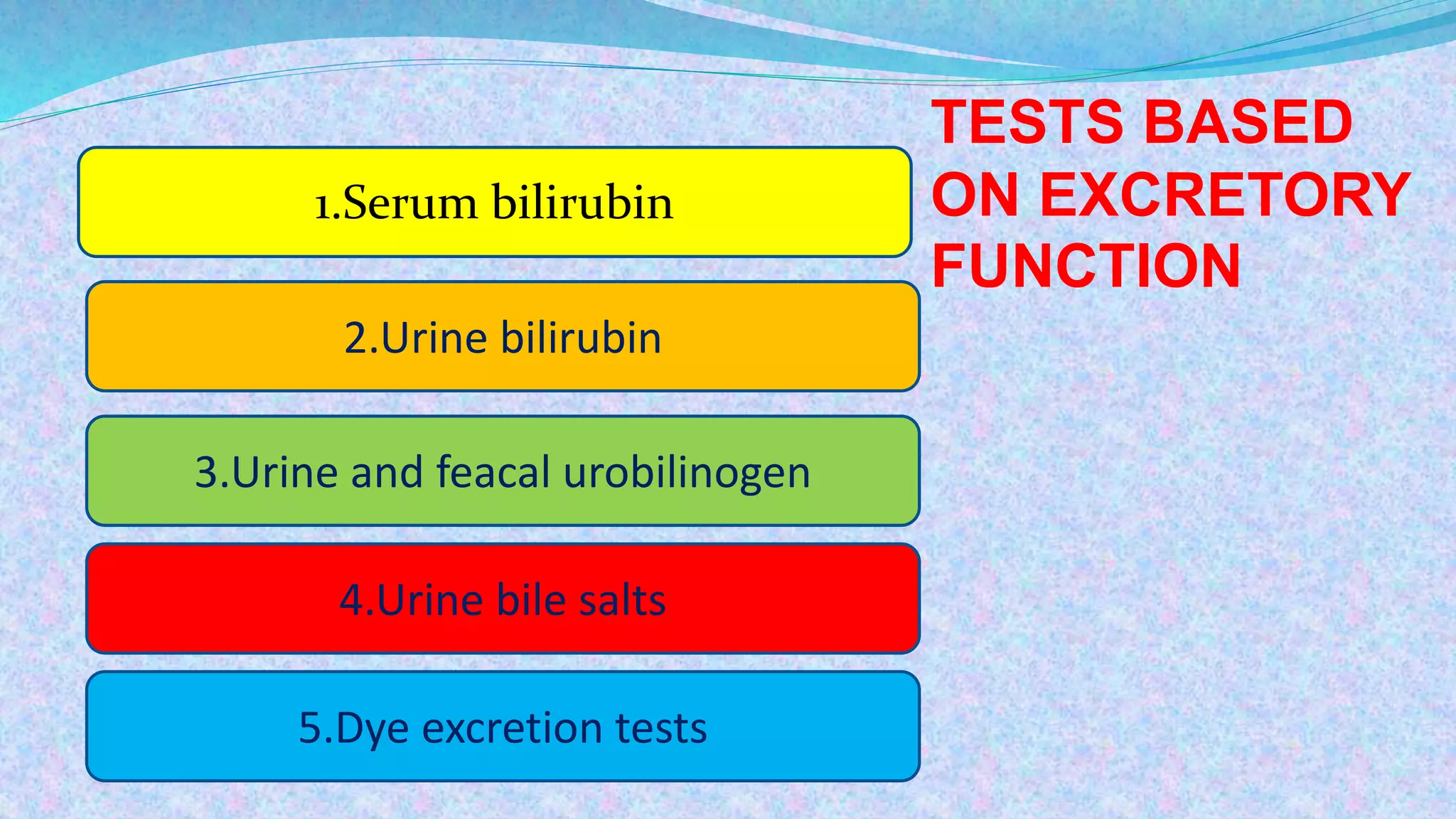
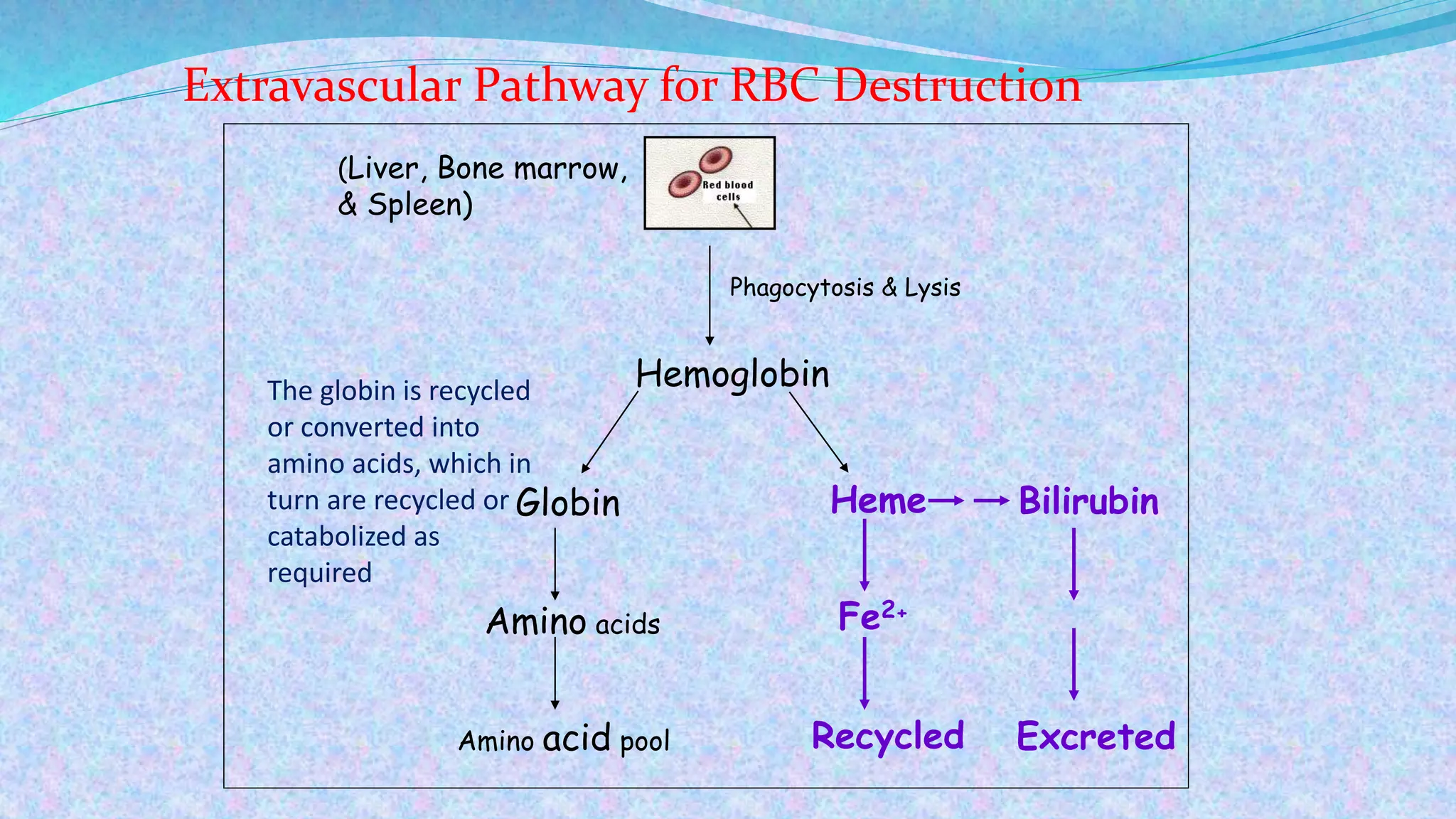
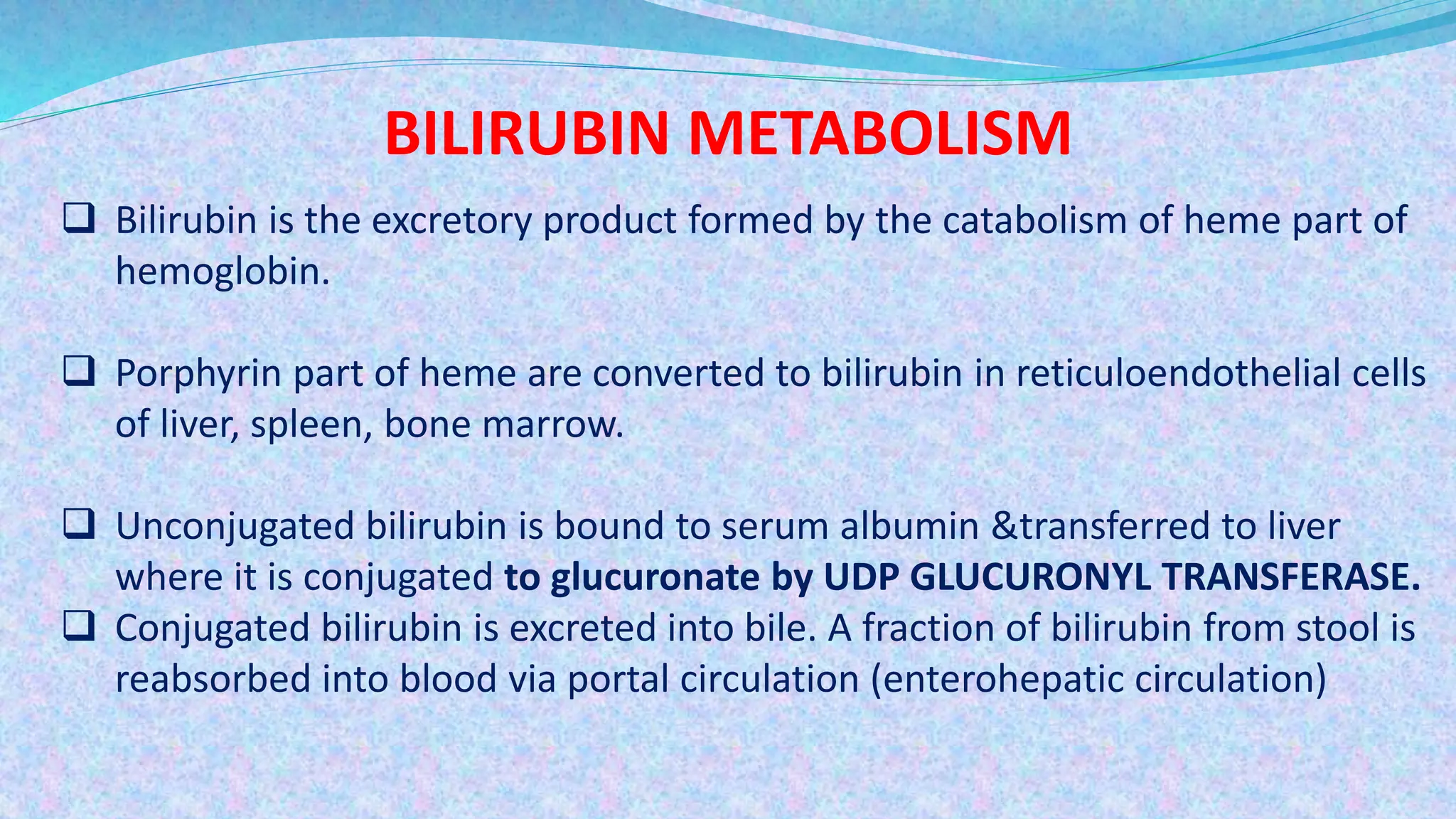
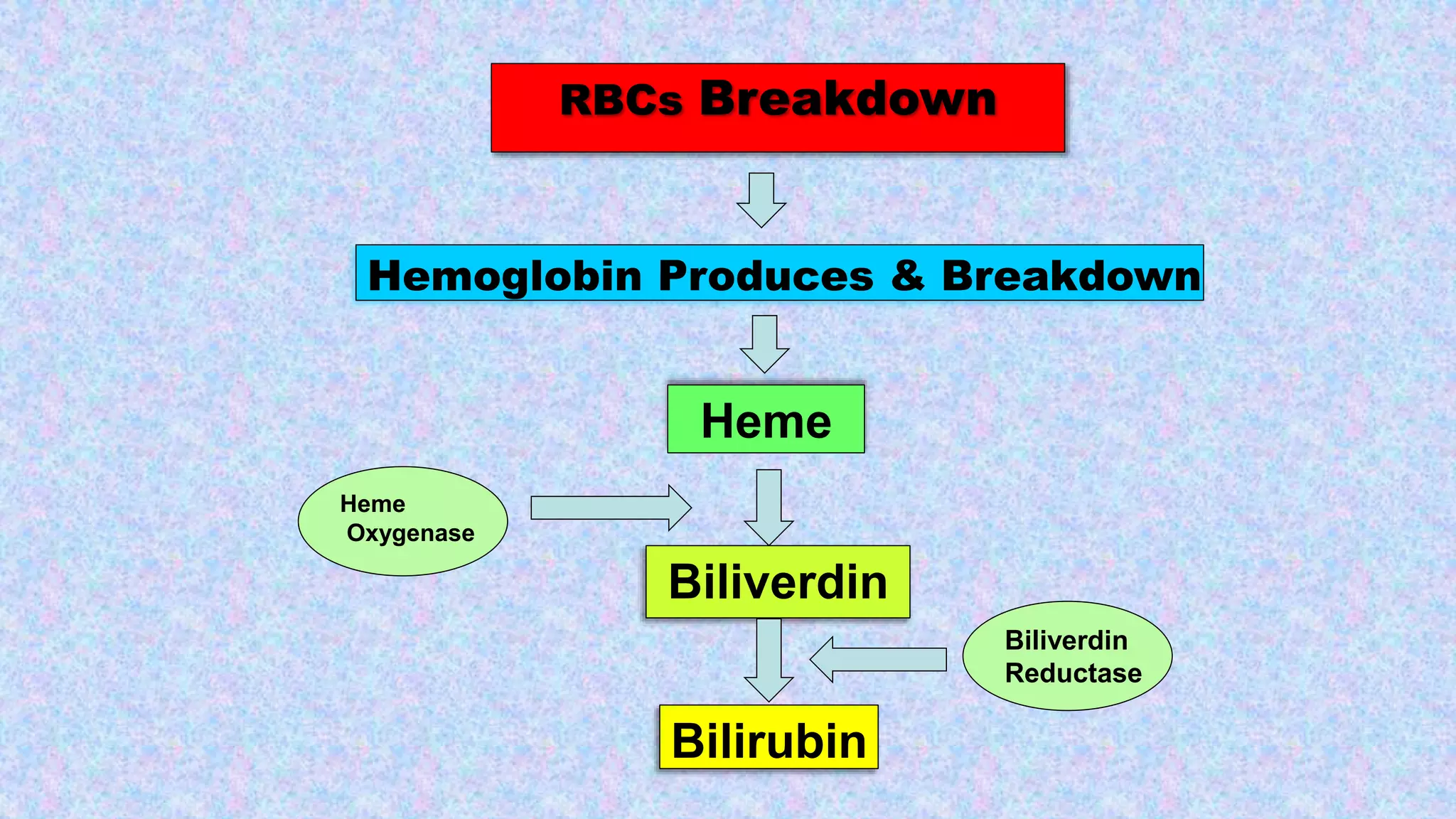
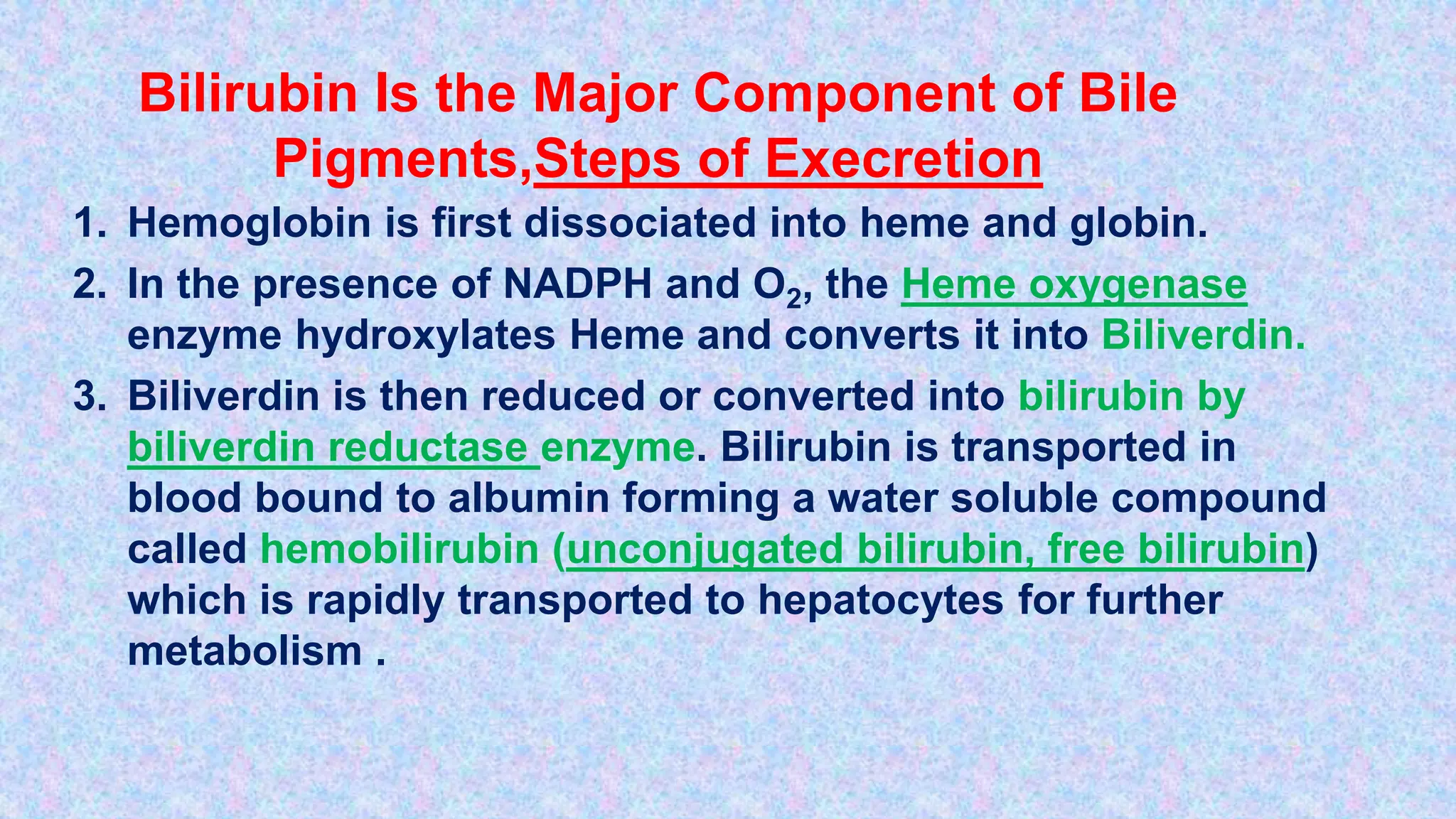
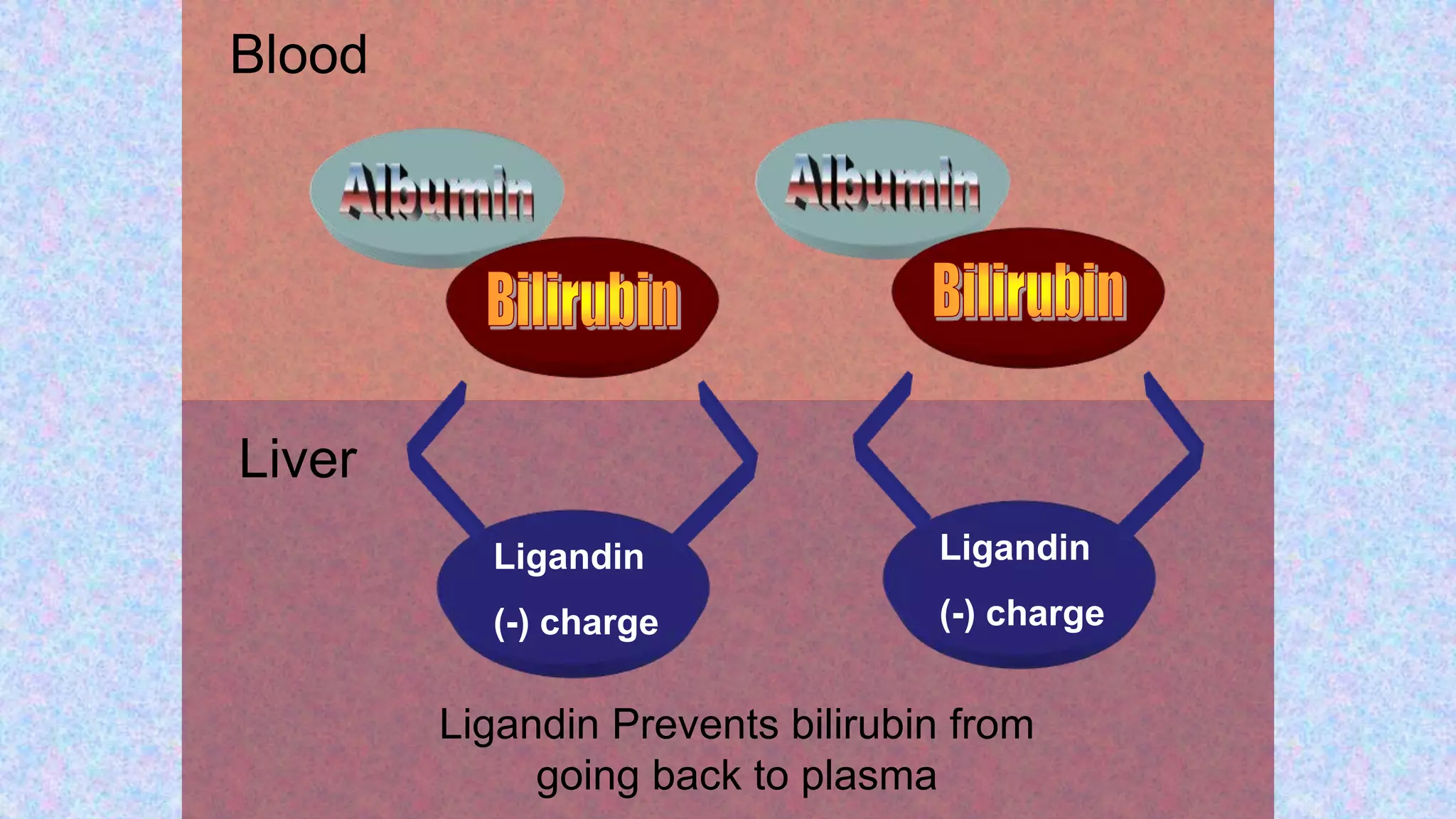
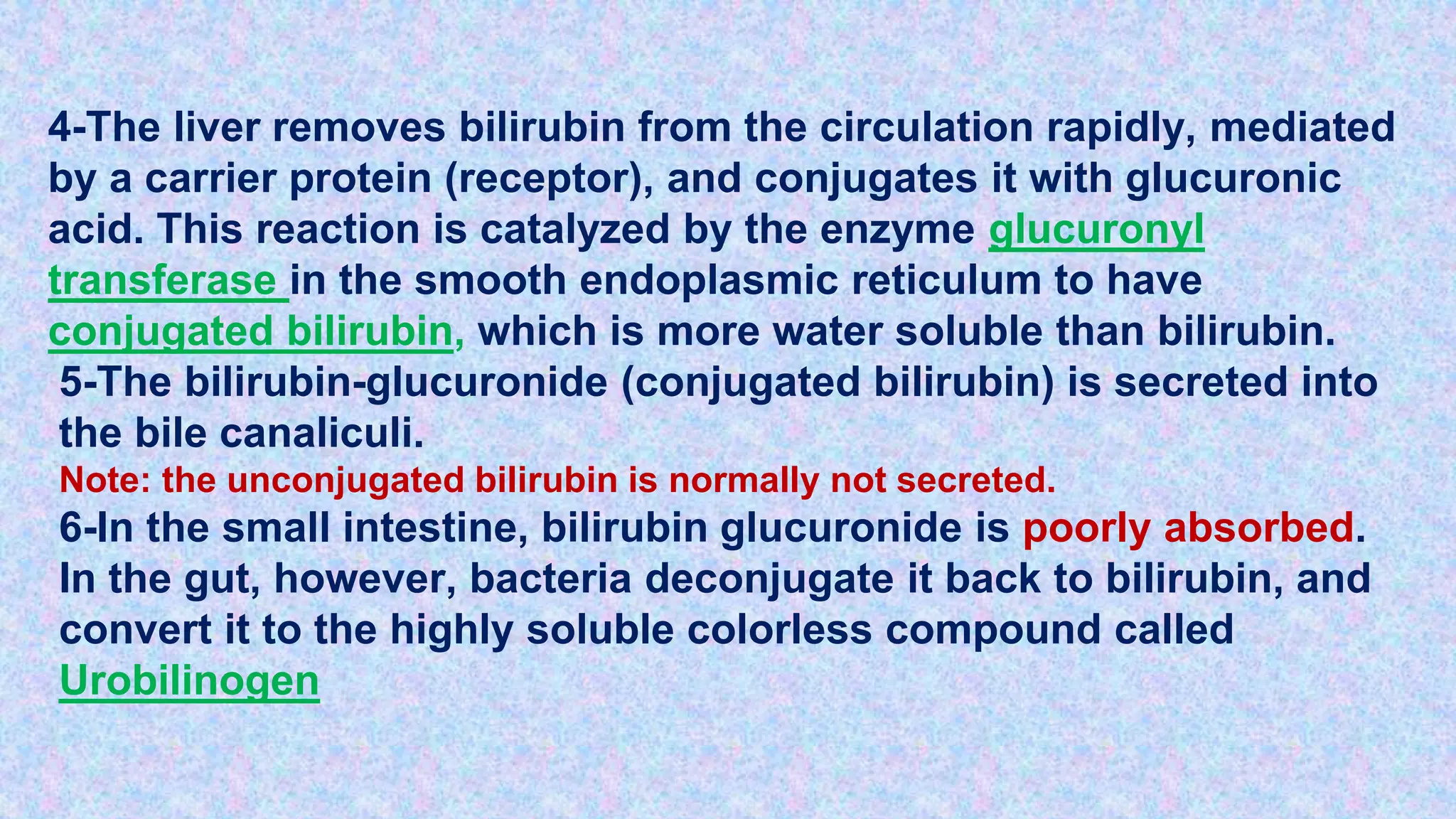
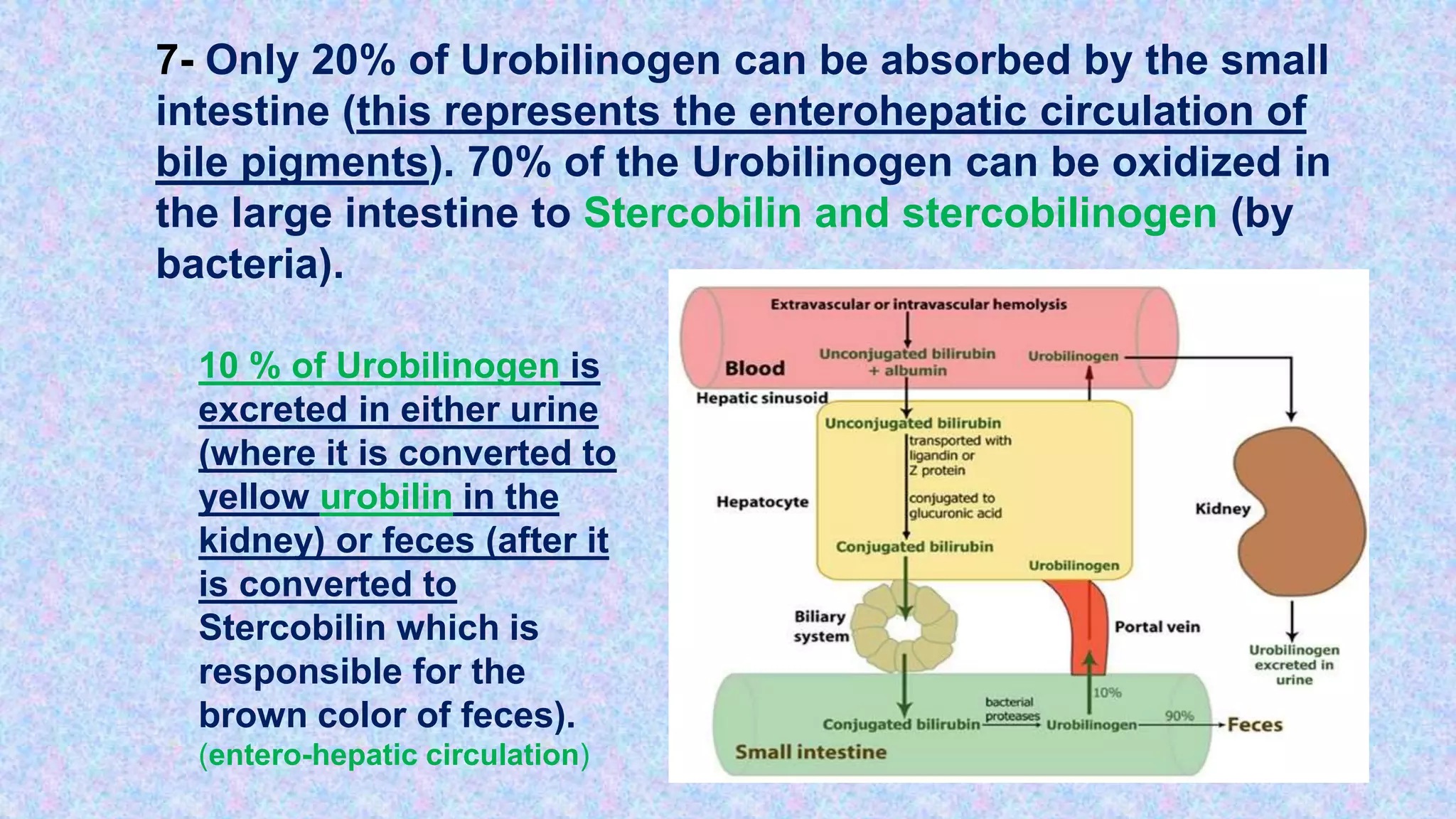
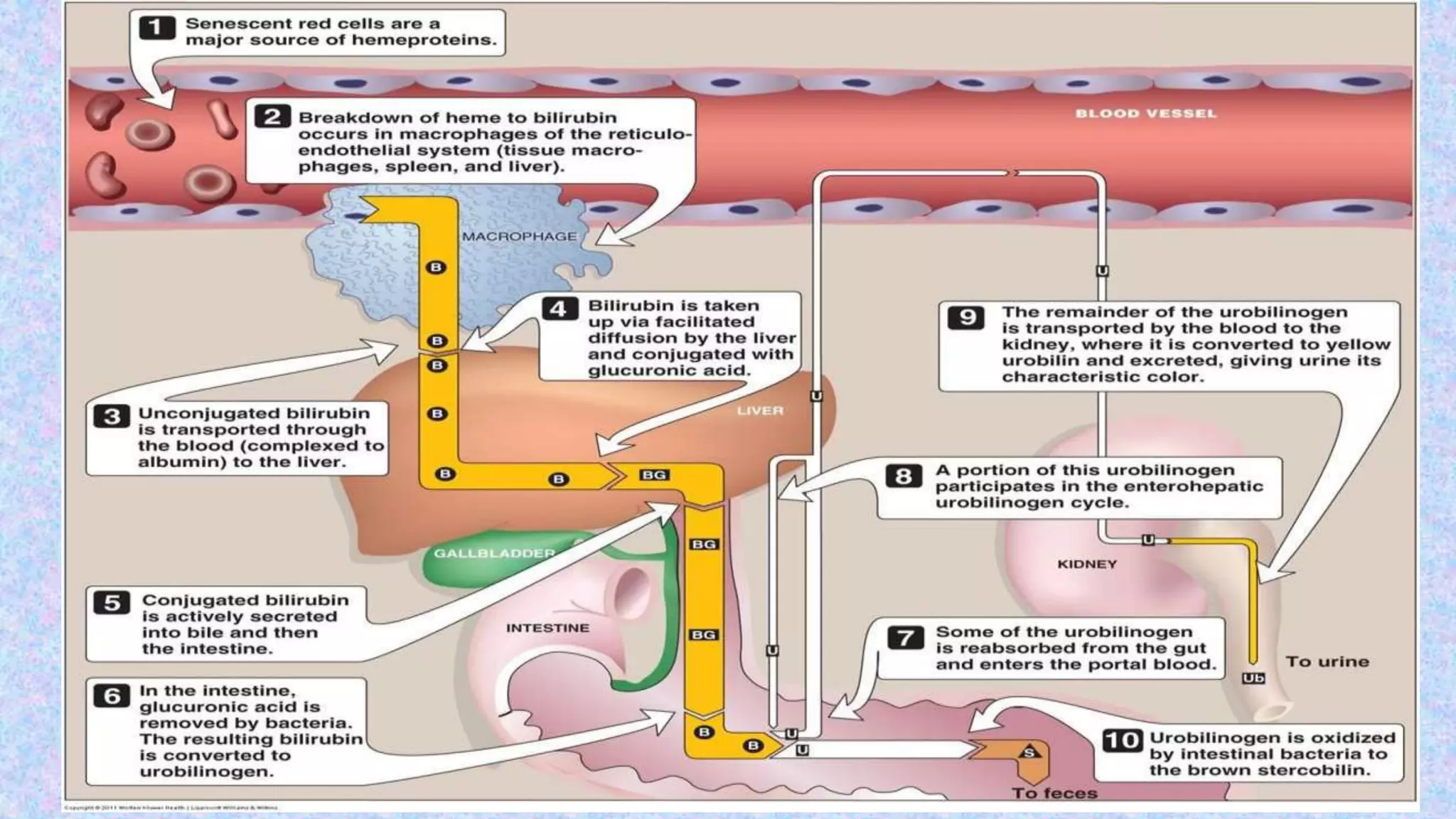
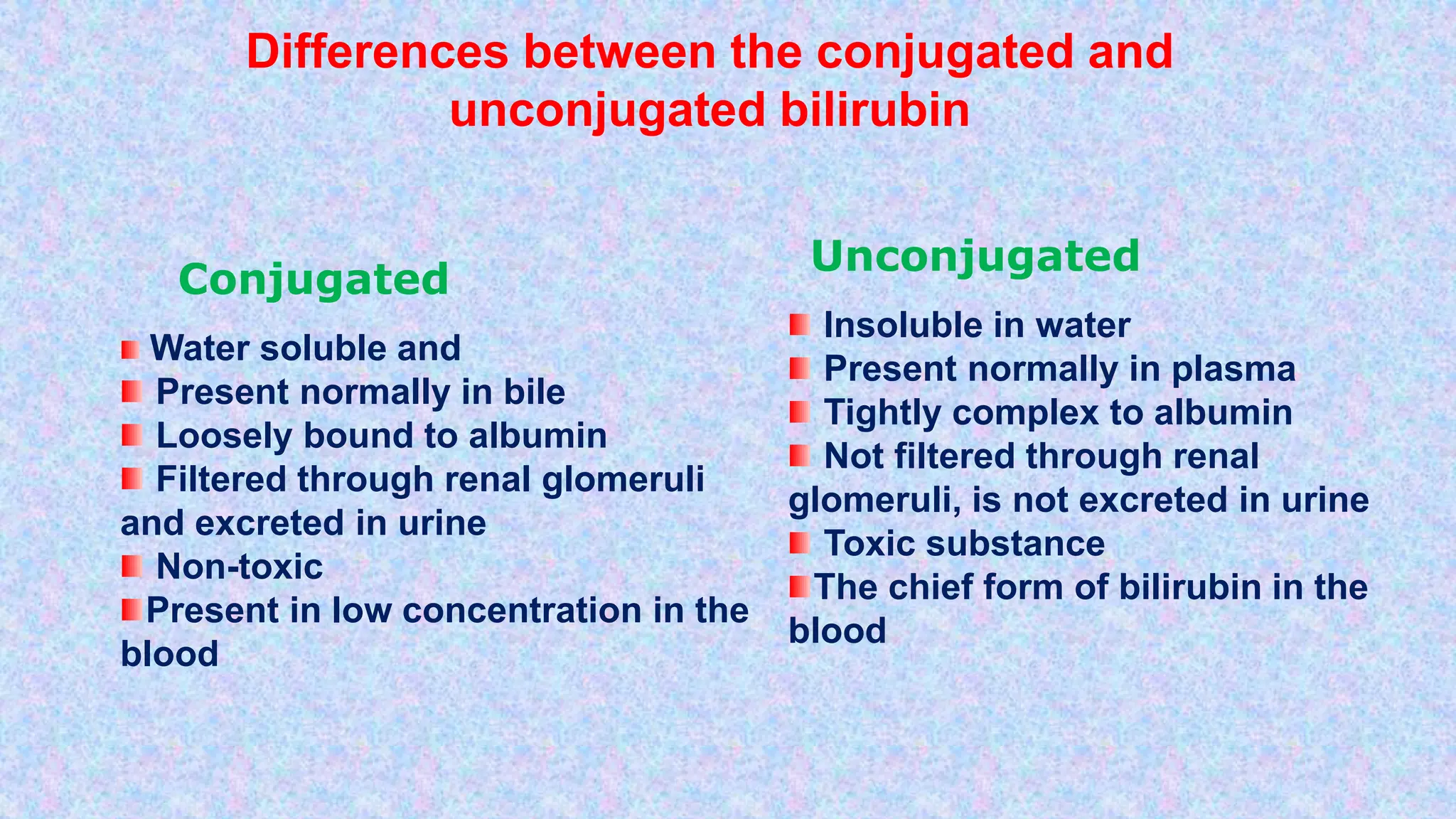
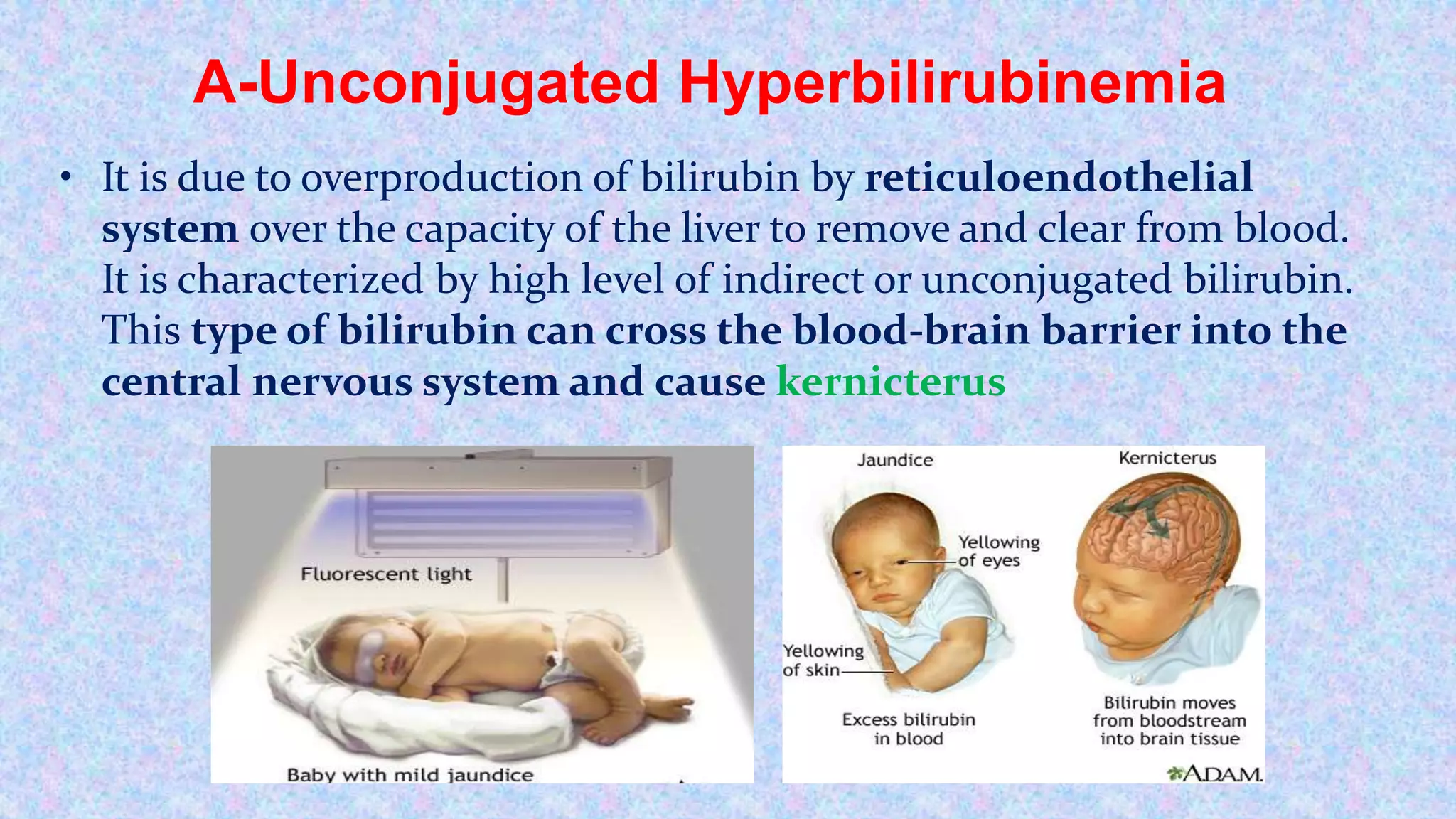
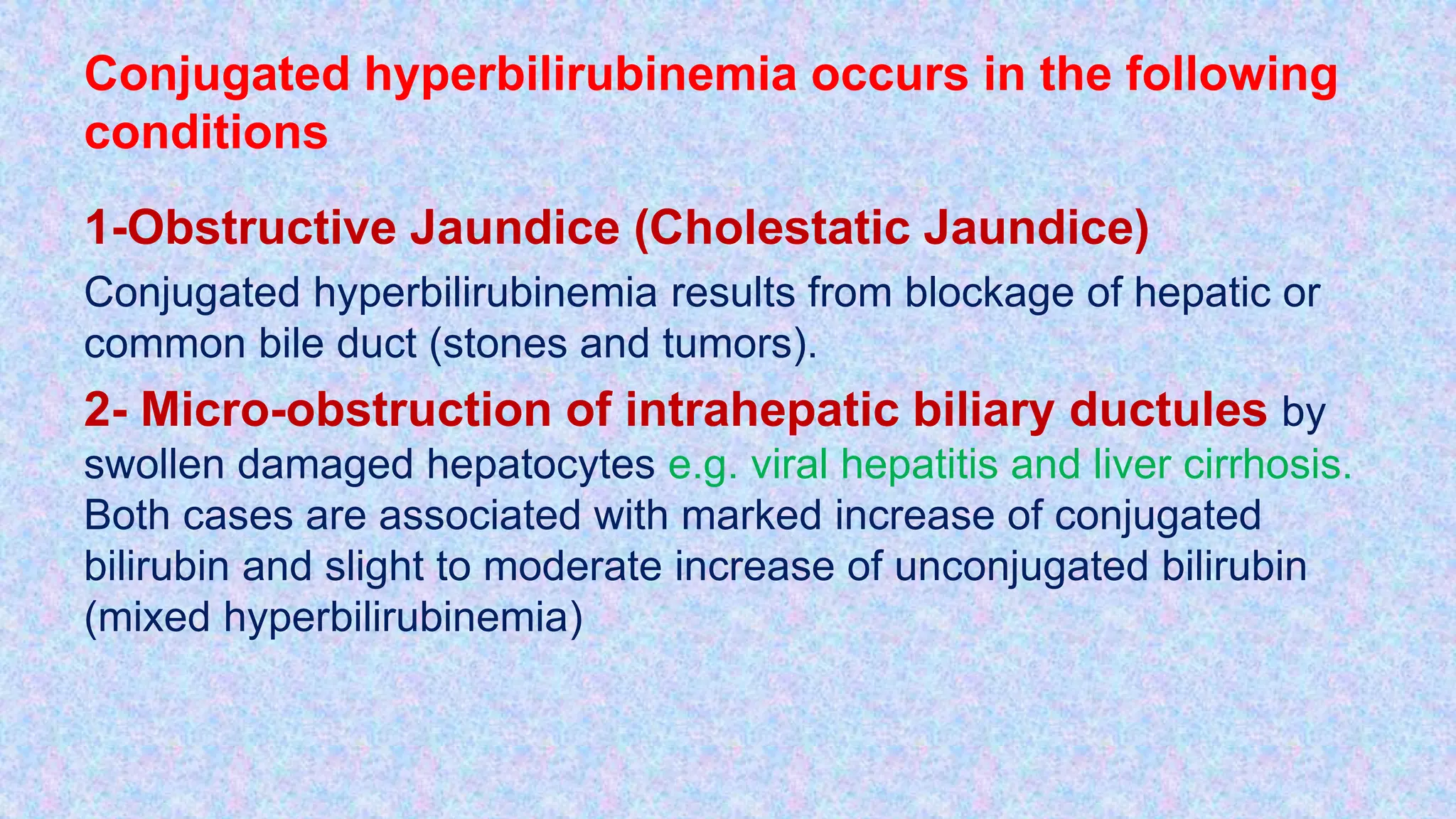
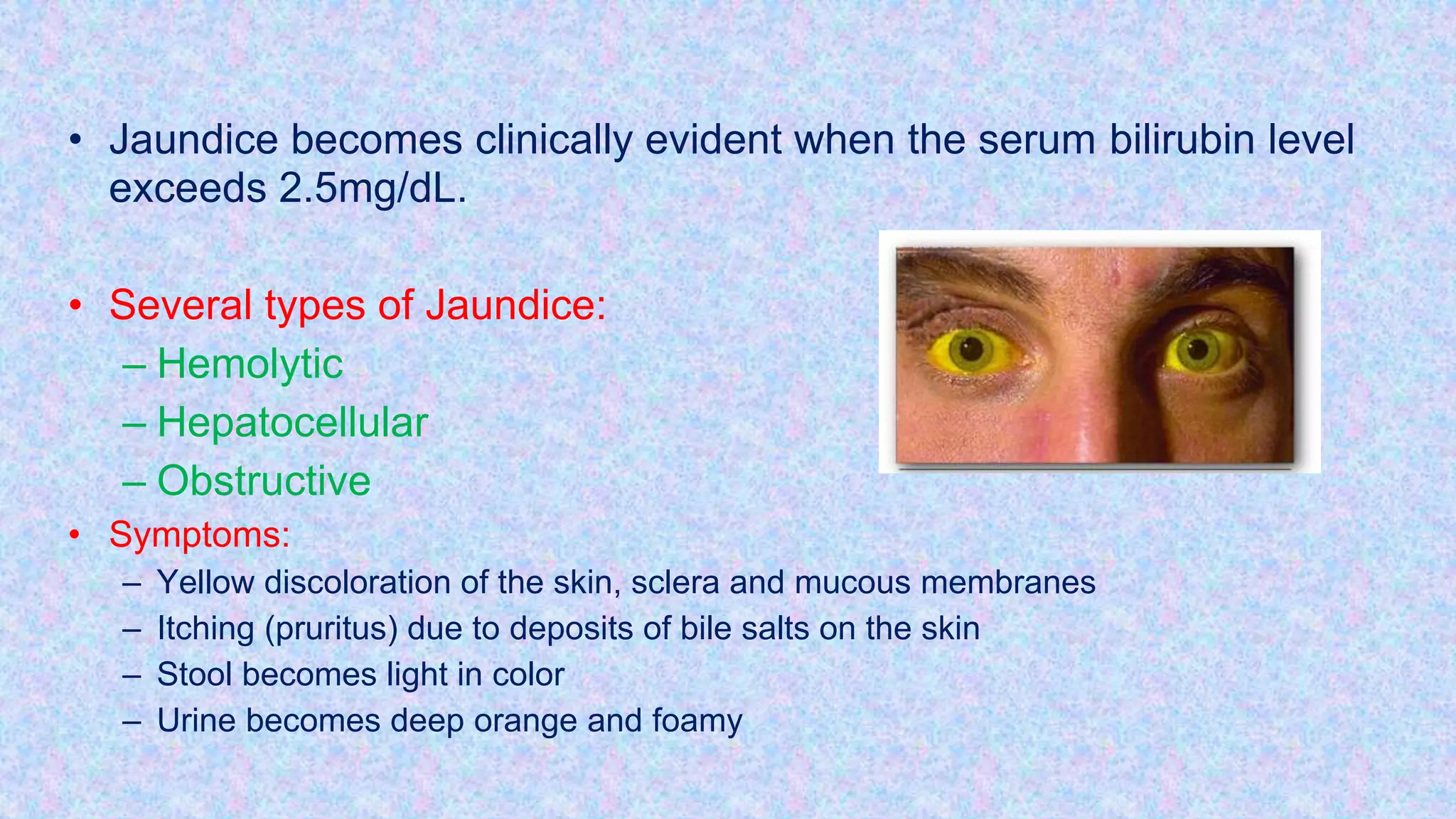
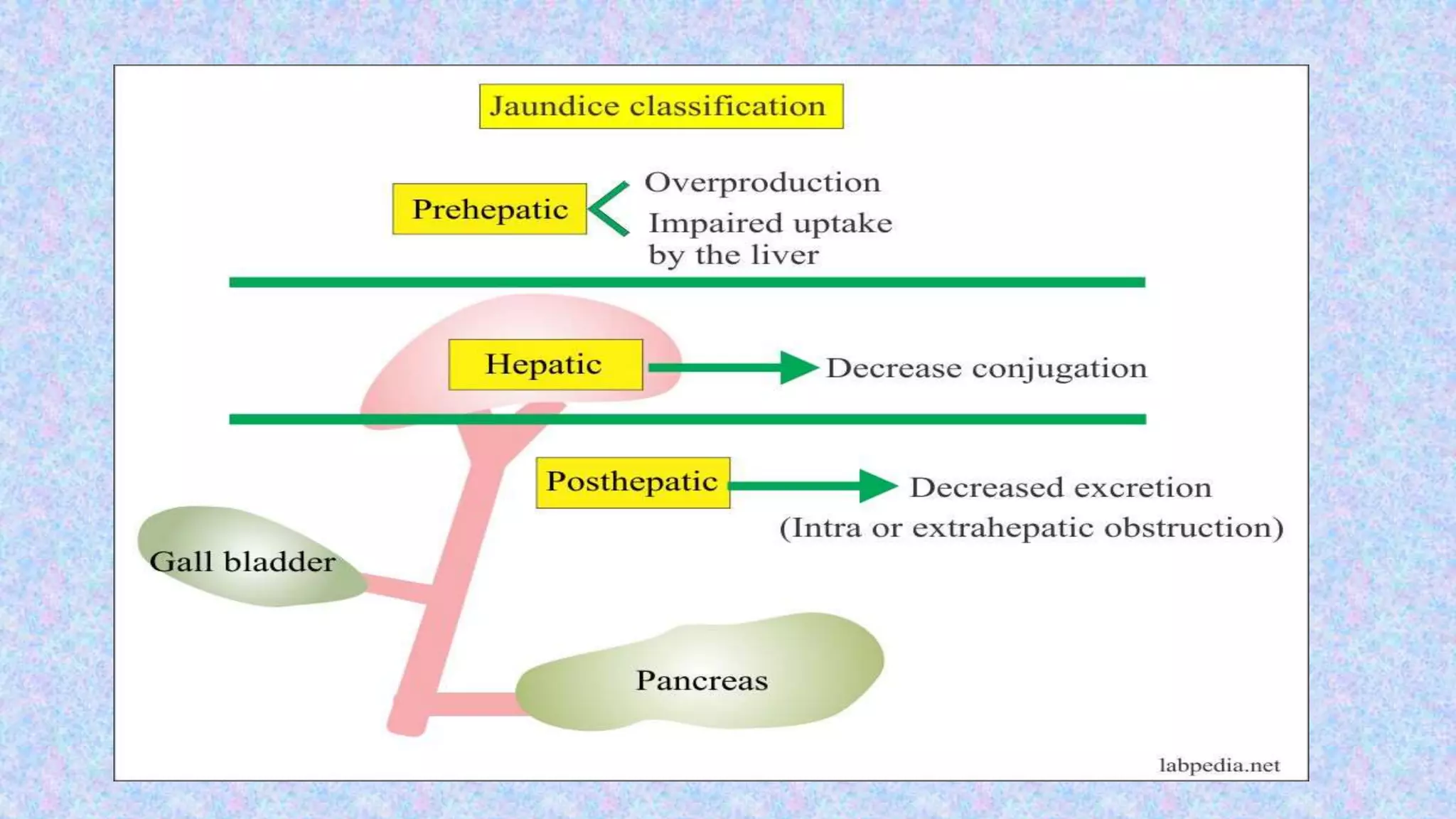
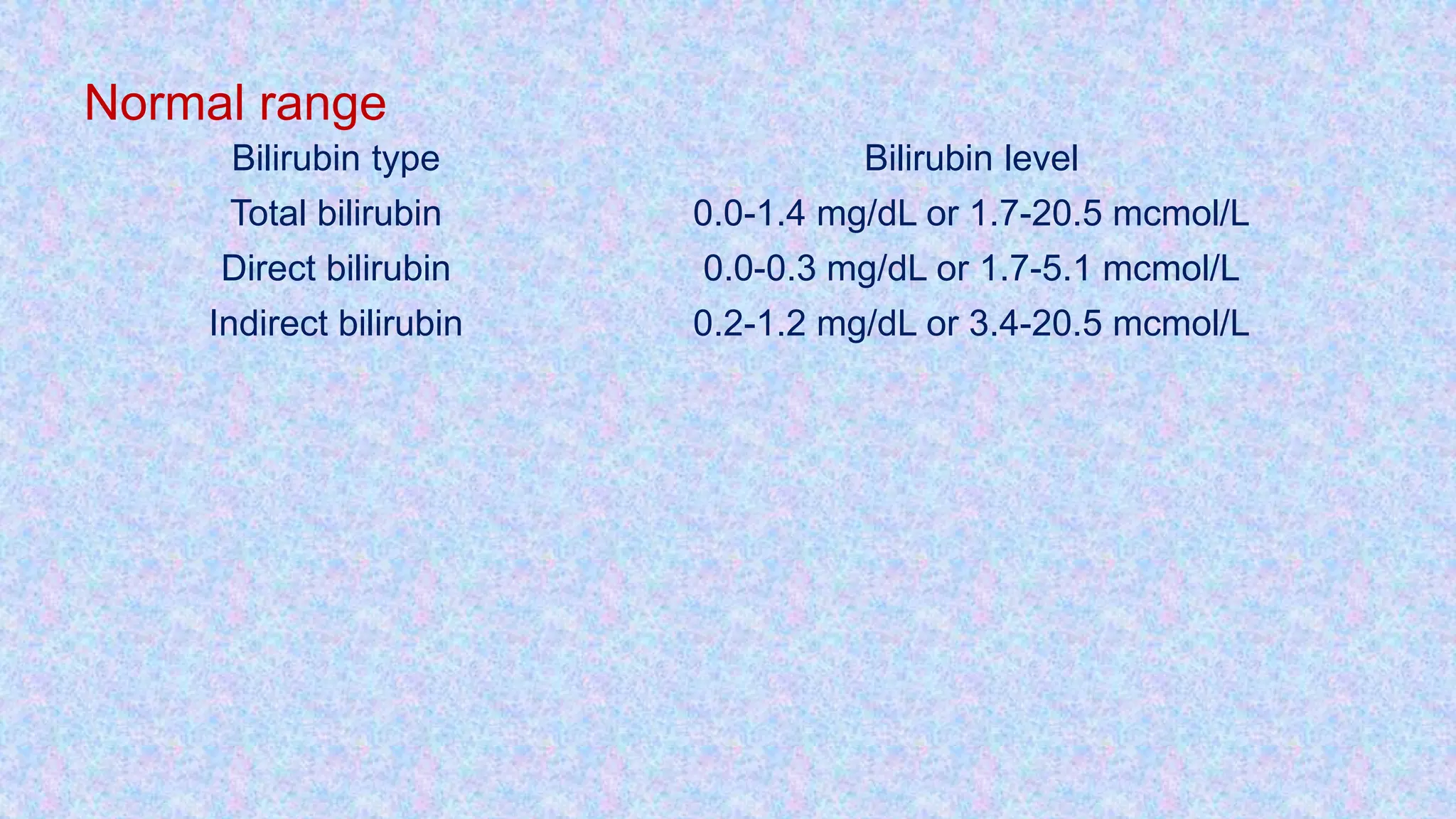
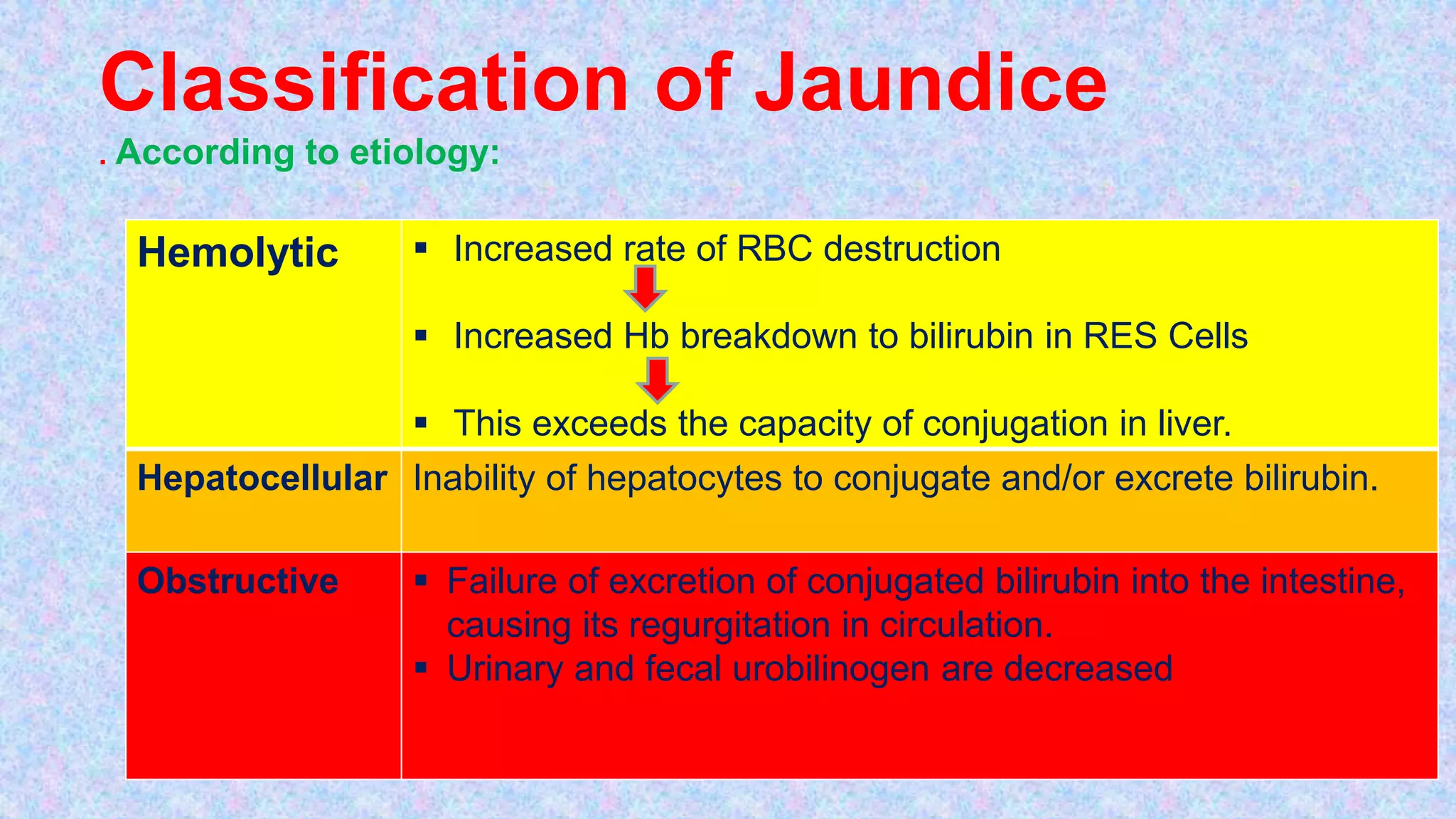
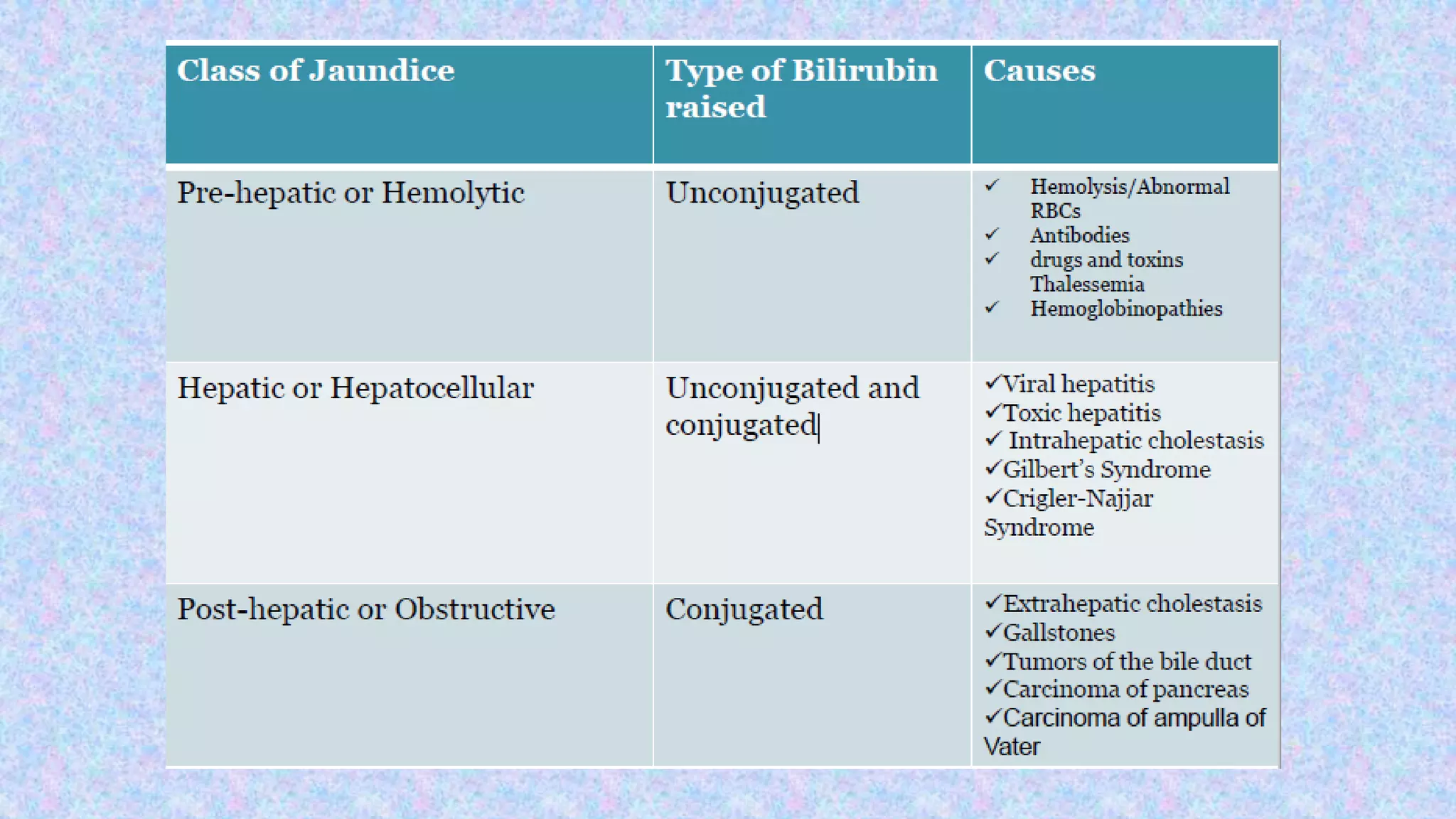
- Bilirubin is produced from the breakdown of heme in red blood cells. The liver conjugates bilirubin so it can be excreted in bile or urine. Elevated bilirubin levels can indicate liver damage or blockages.
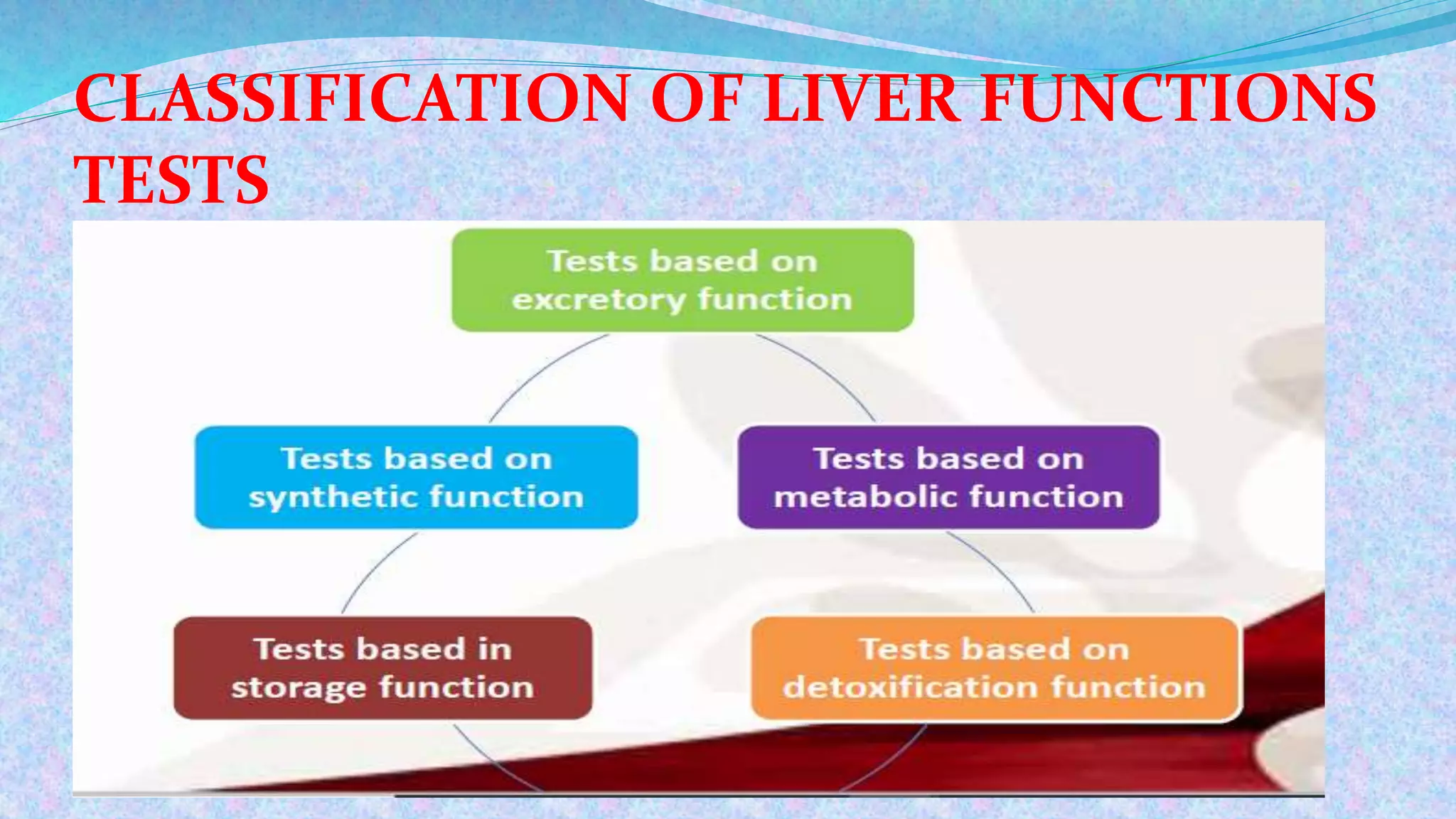
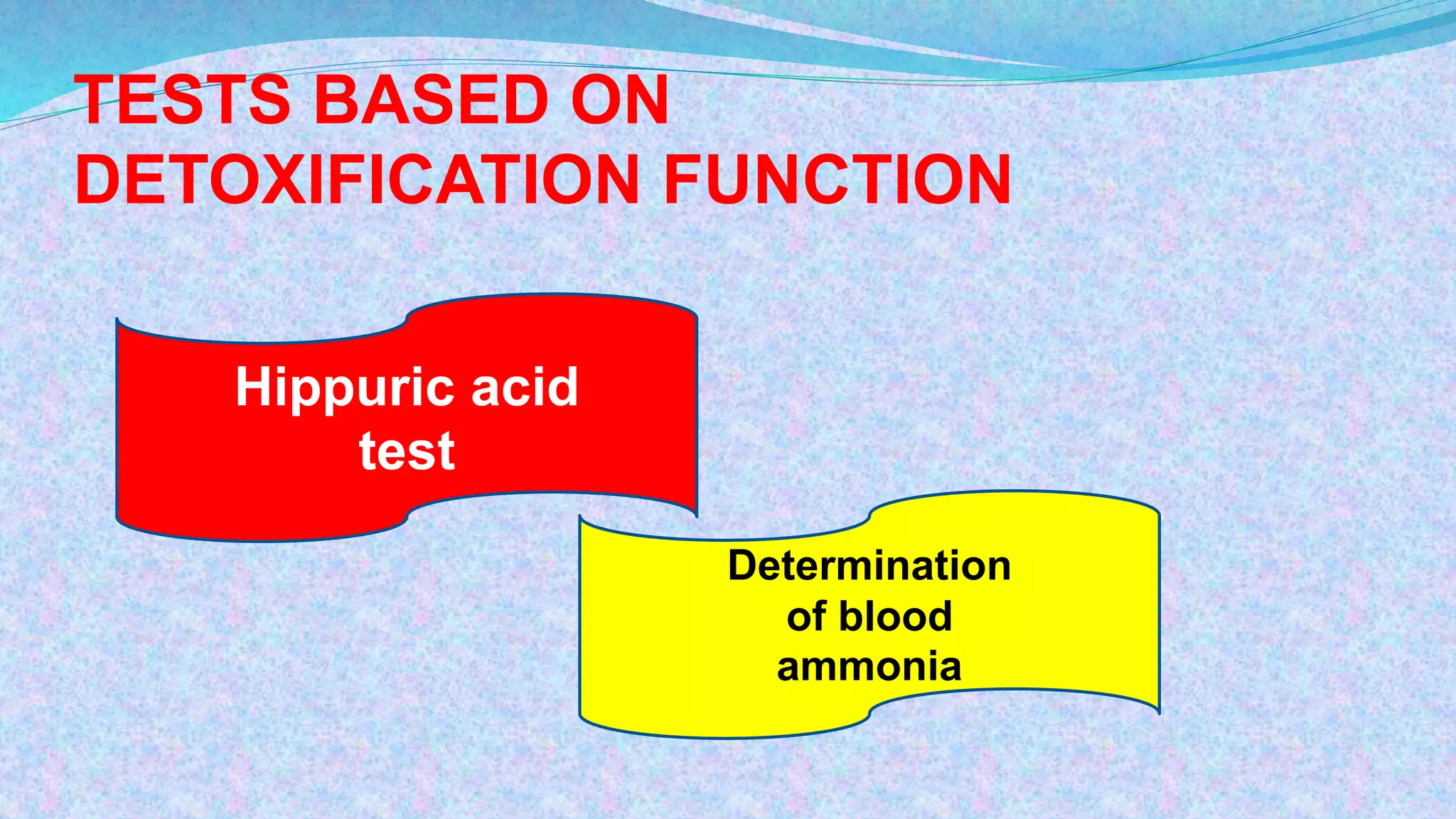
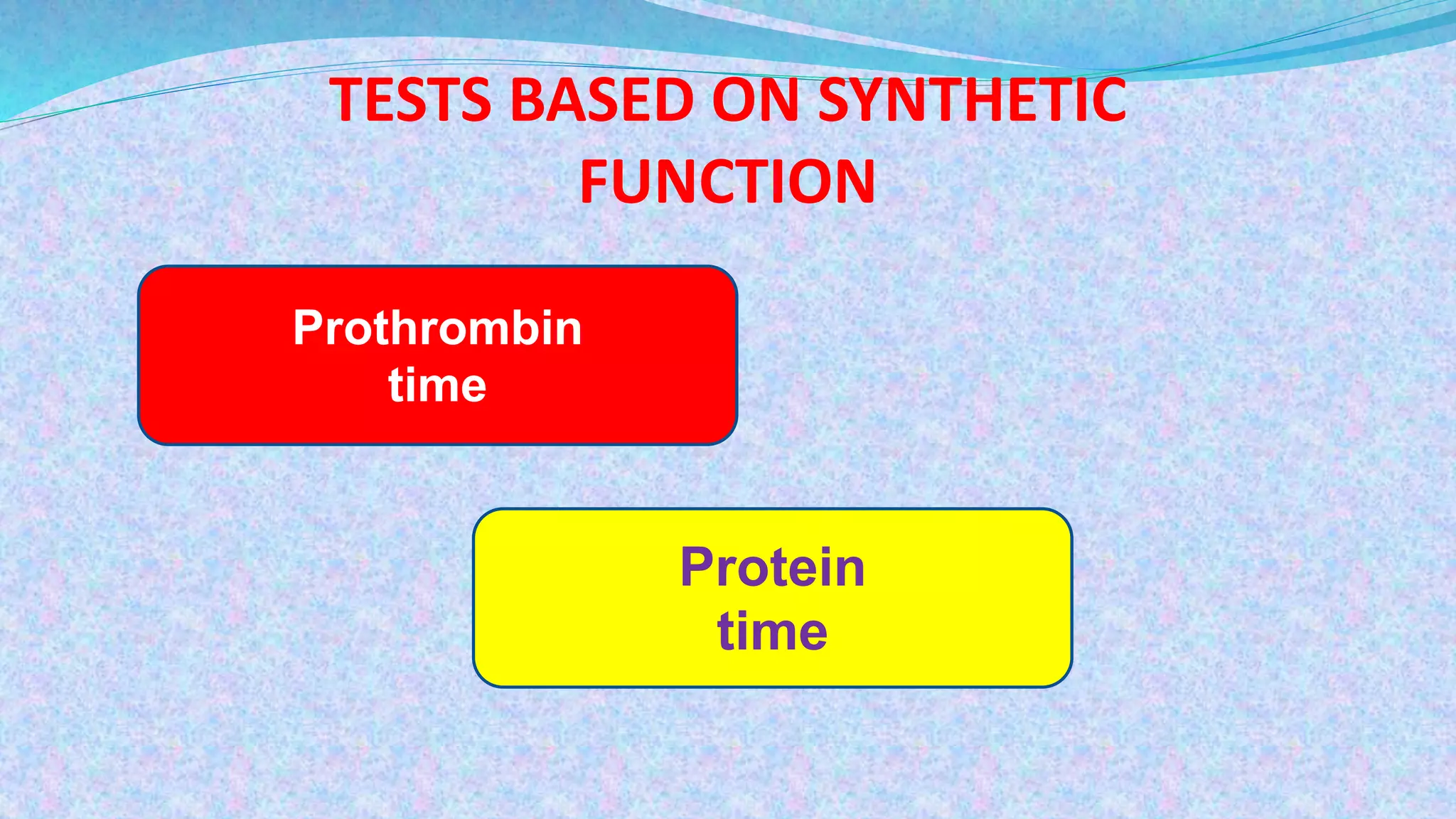
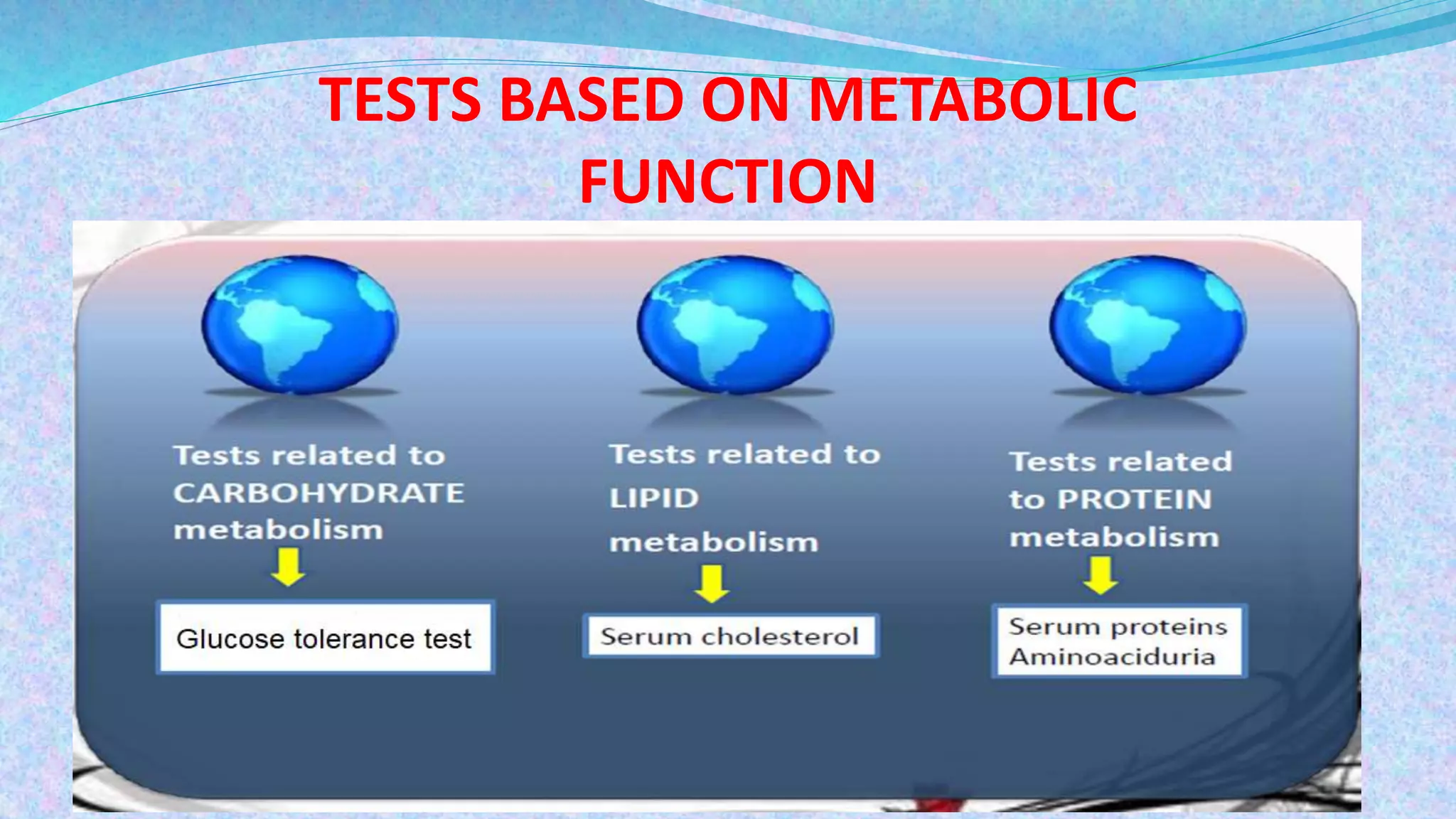
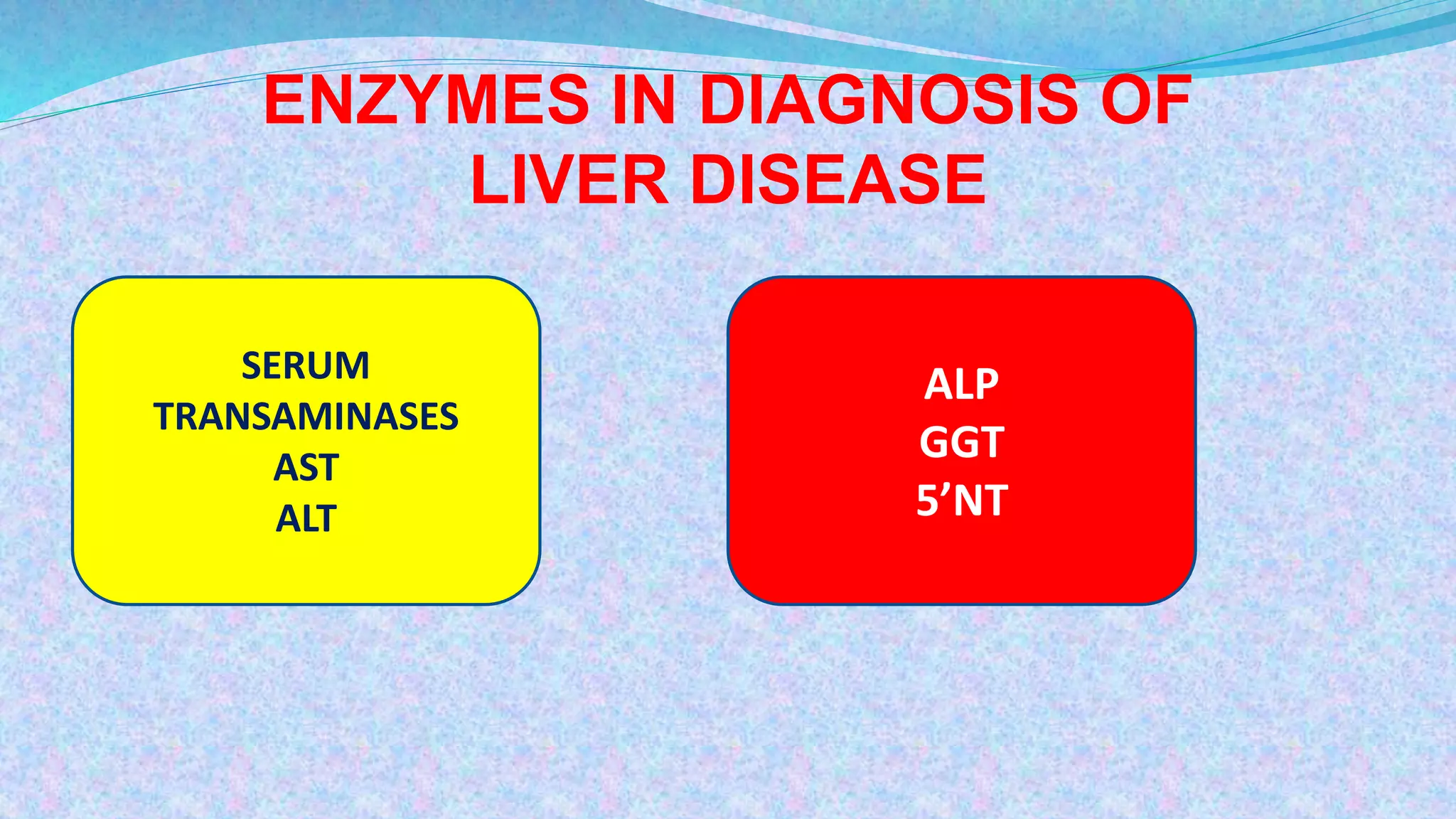
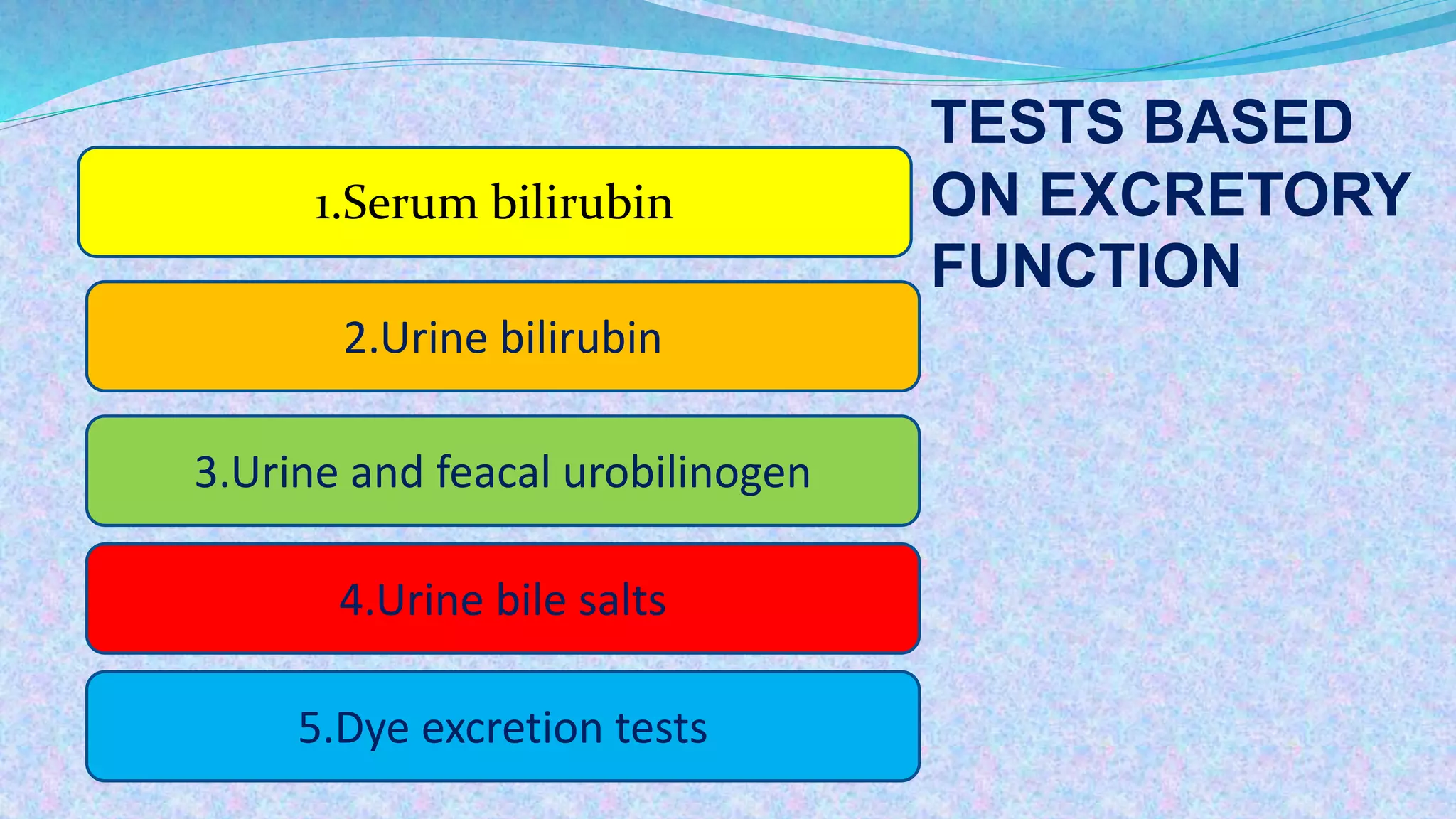
- Tests are classified based on the liver's excretory, detoxification, synthetic and metabolic functions. Enzymes like AST, ALT and GGT are also measured