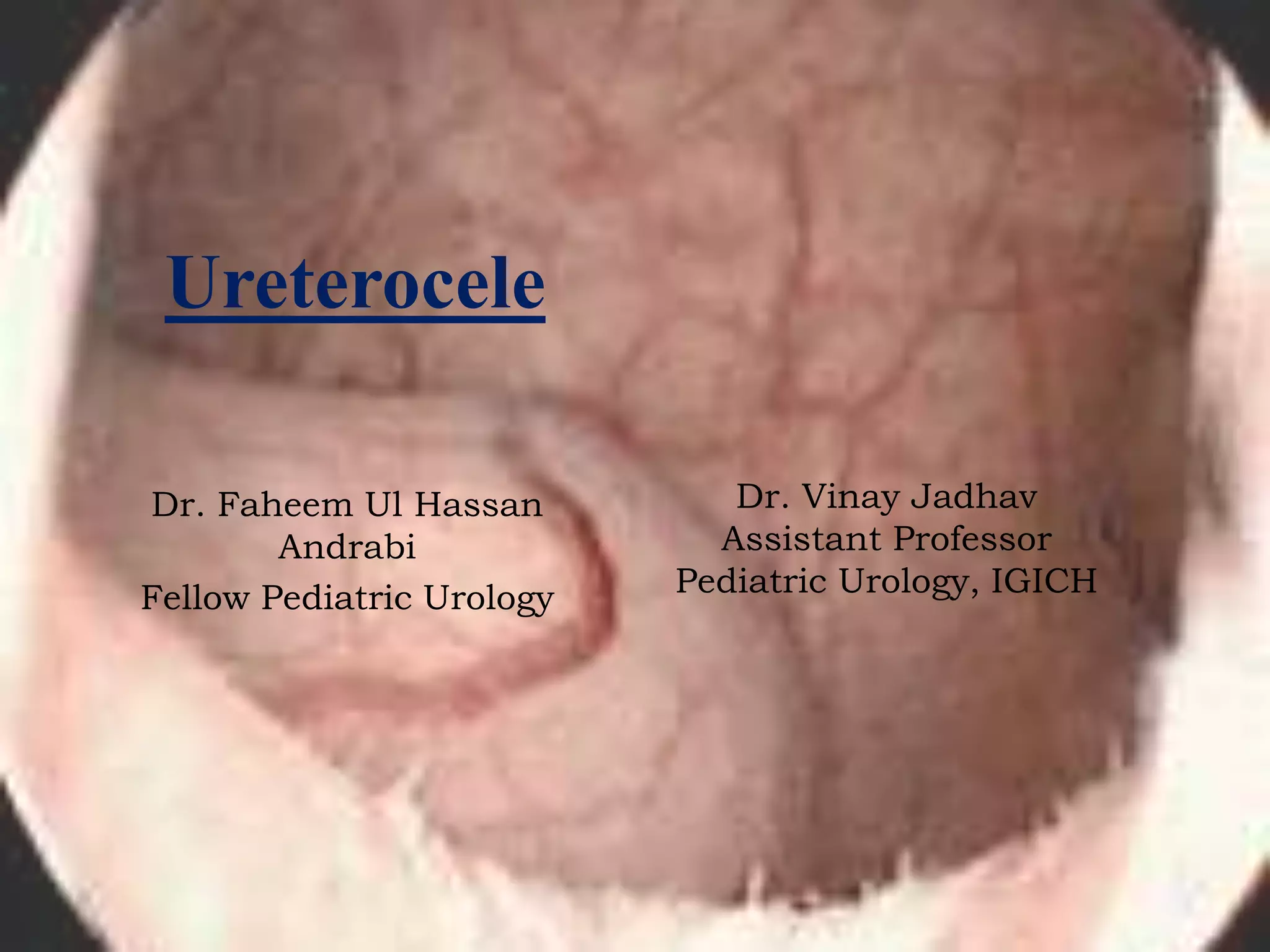
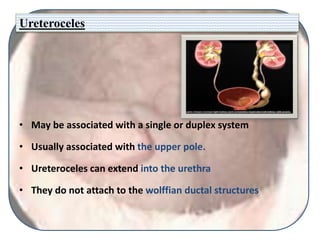
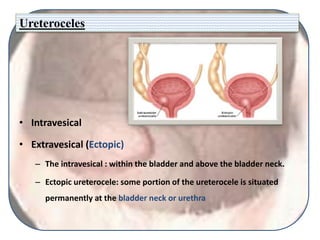
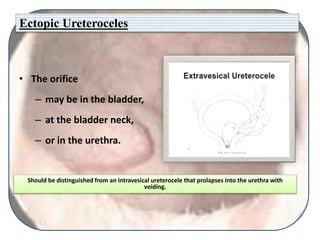
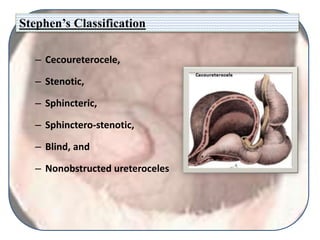
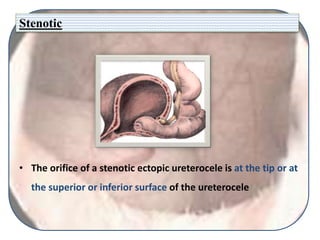
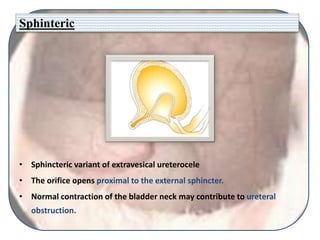
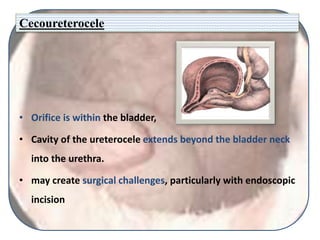
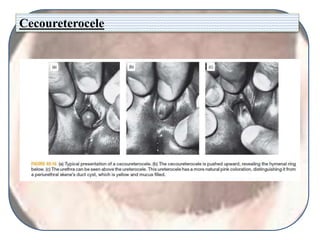
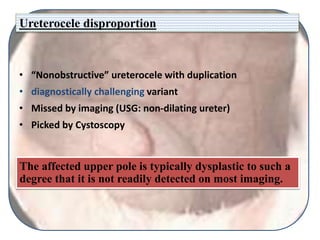
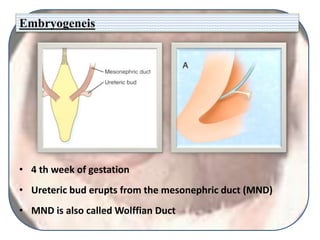
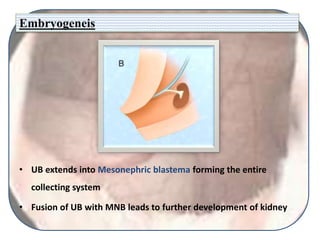
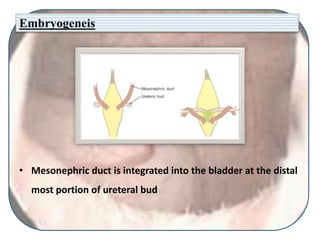
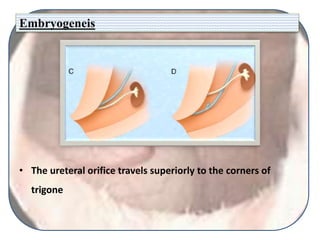
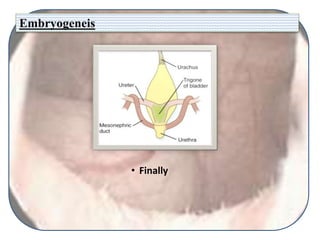
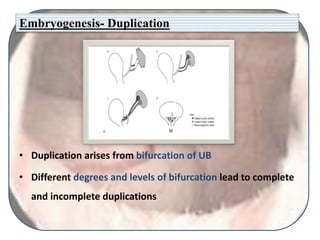
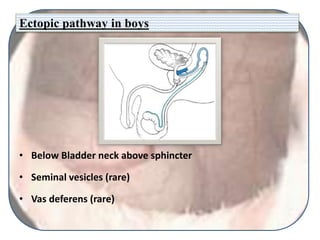
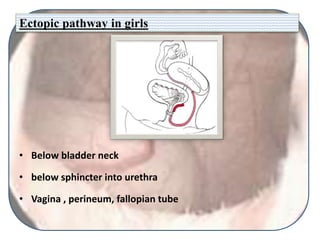
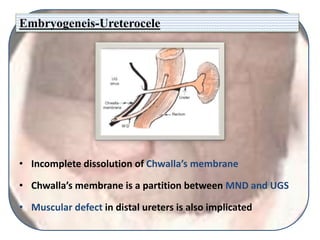
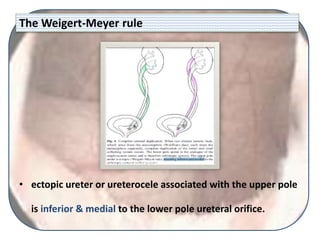
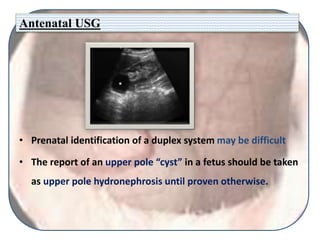
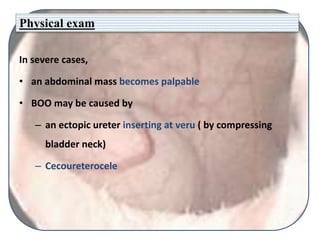
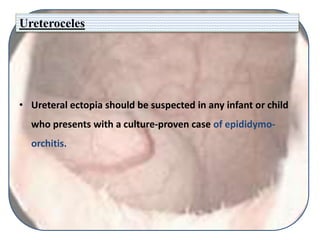
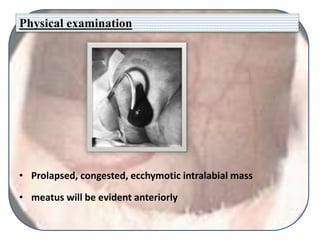
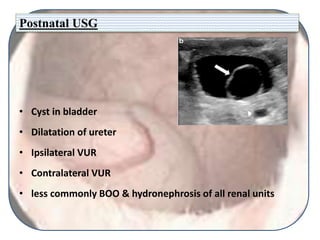
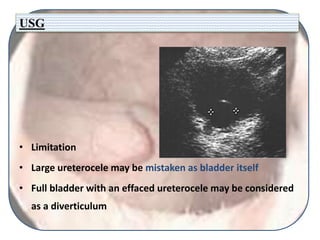
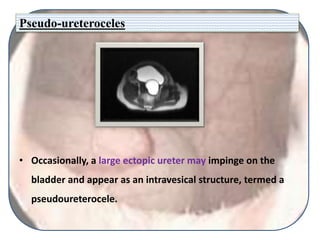
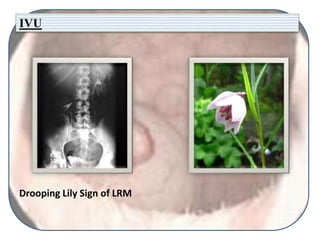
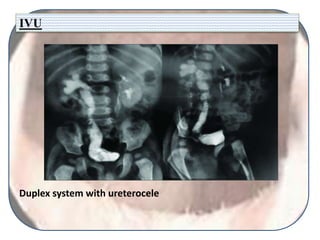
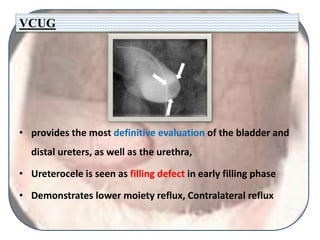
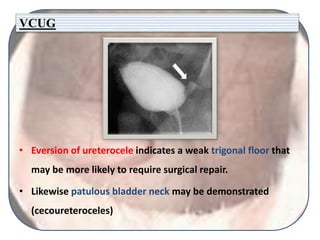
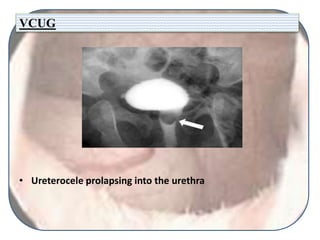
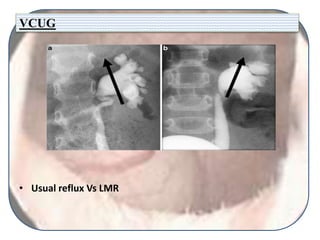
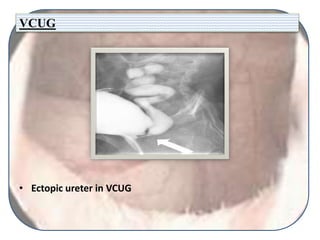
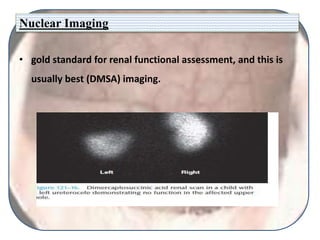
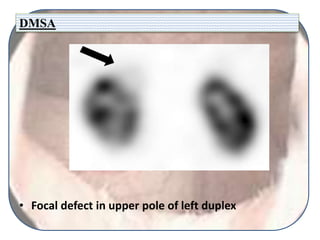
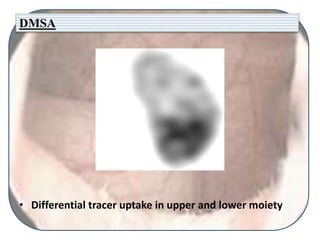
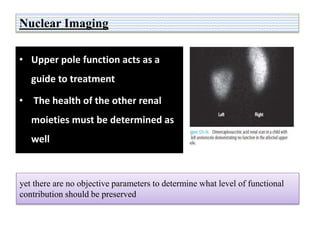
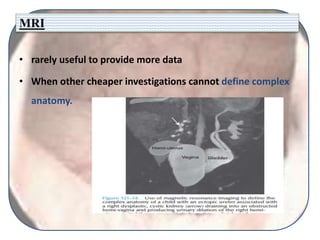
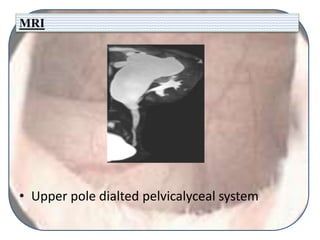
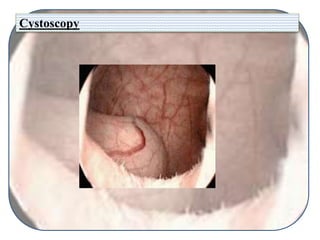
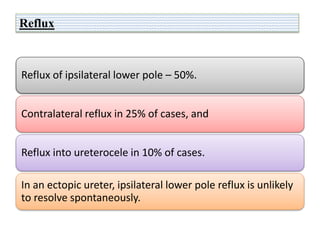
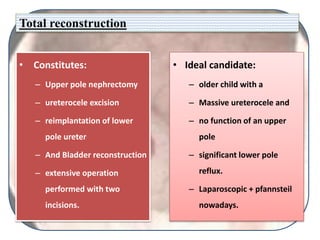
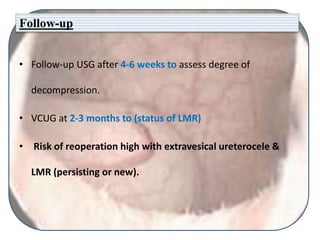
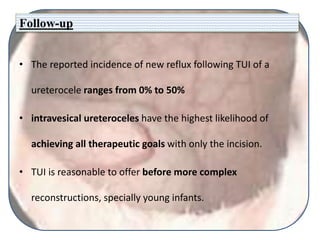
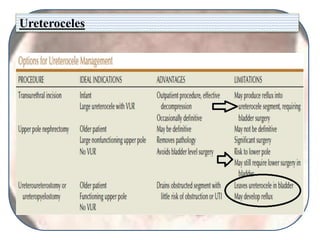
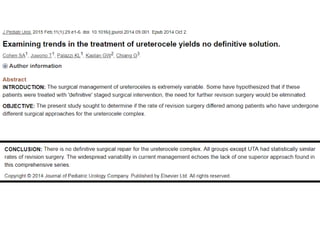
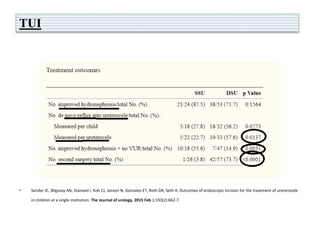
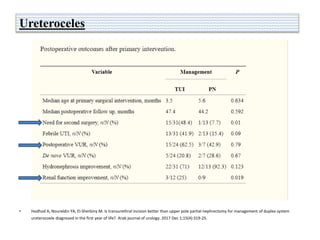
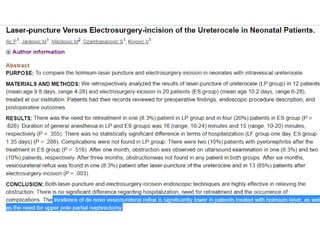
This document discusses ureteroceles, which are cystic dilations of the distal ureter that may be associated with defects in ureteral maturation. Ureteroceles can be intravesical, extending into the bladder, or extravesical/ectopic, extending beyond the bladder neck. They are usually associated with the upper renal moiety in a duplex system. Clinical presentations include infections, incontinence, pain, or being found incidentally. Diagnostic imaging includes ultrasound, IVU, VCUG, nuclear medicine scans, and cystoscopy. Management goals are preserving renal function, eliminating obstruction/reflux, and continence. Treatment depends on individual factors and may include observation, acute decomp