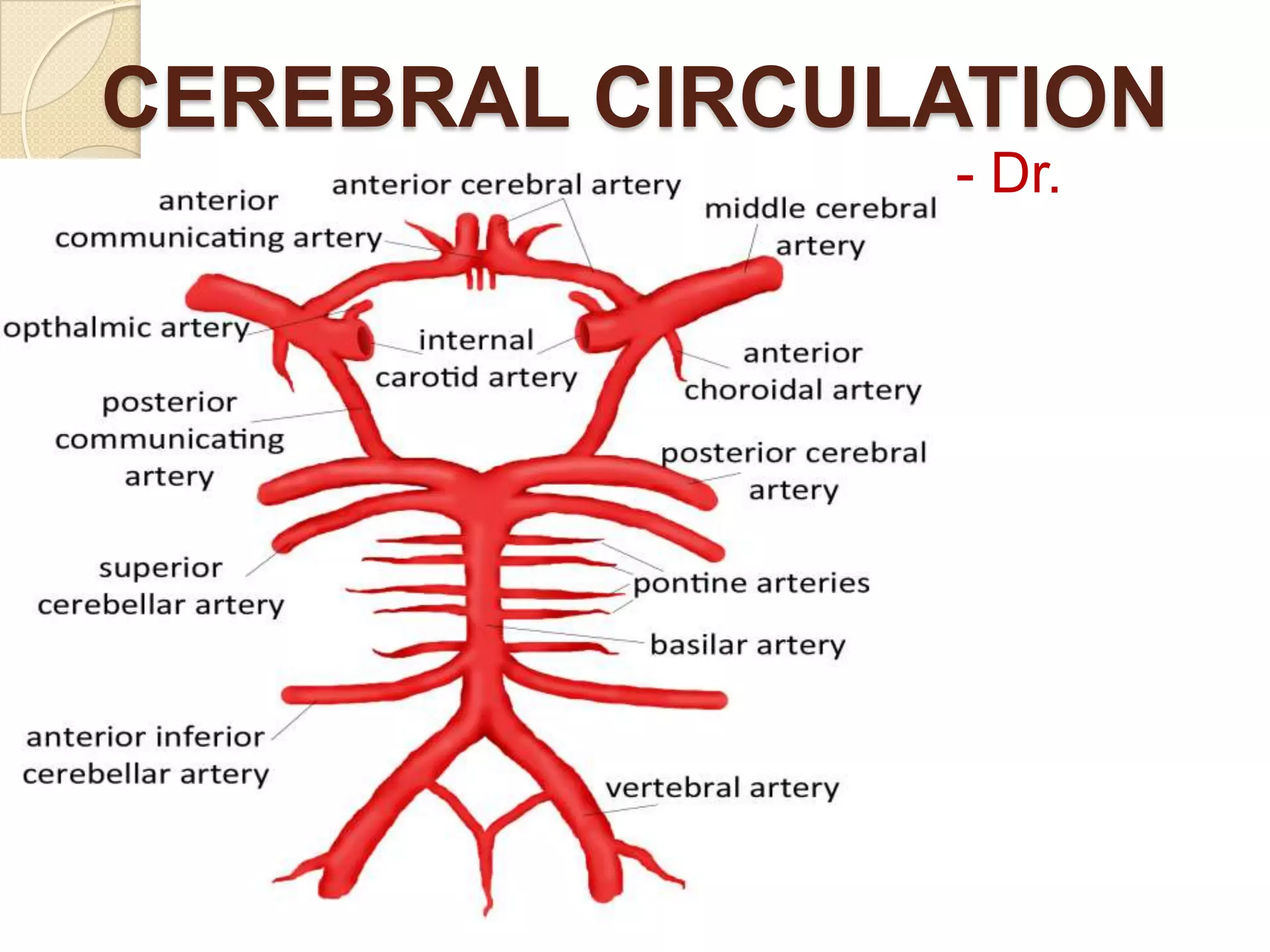
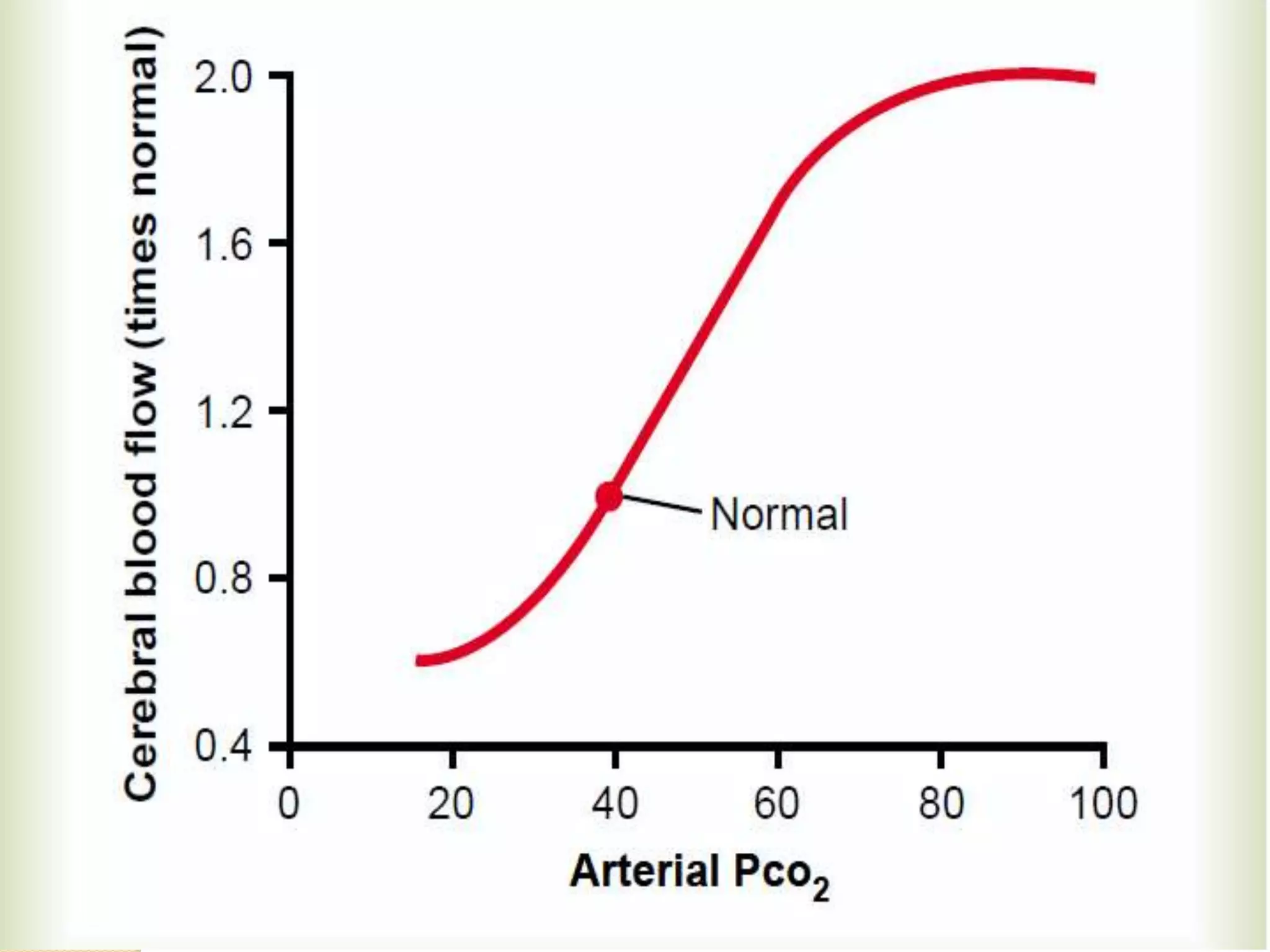
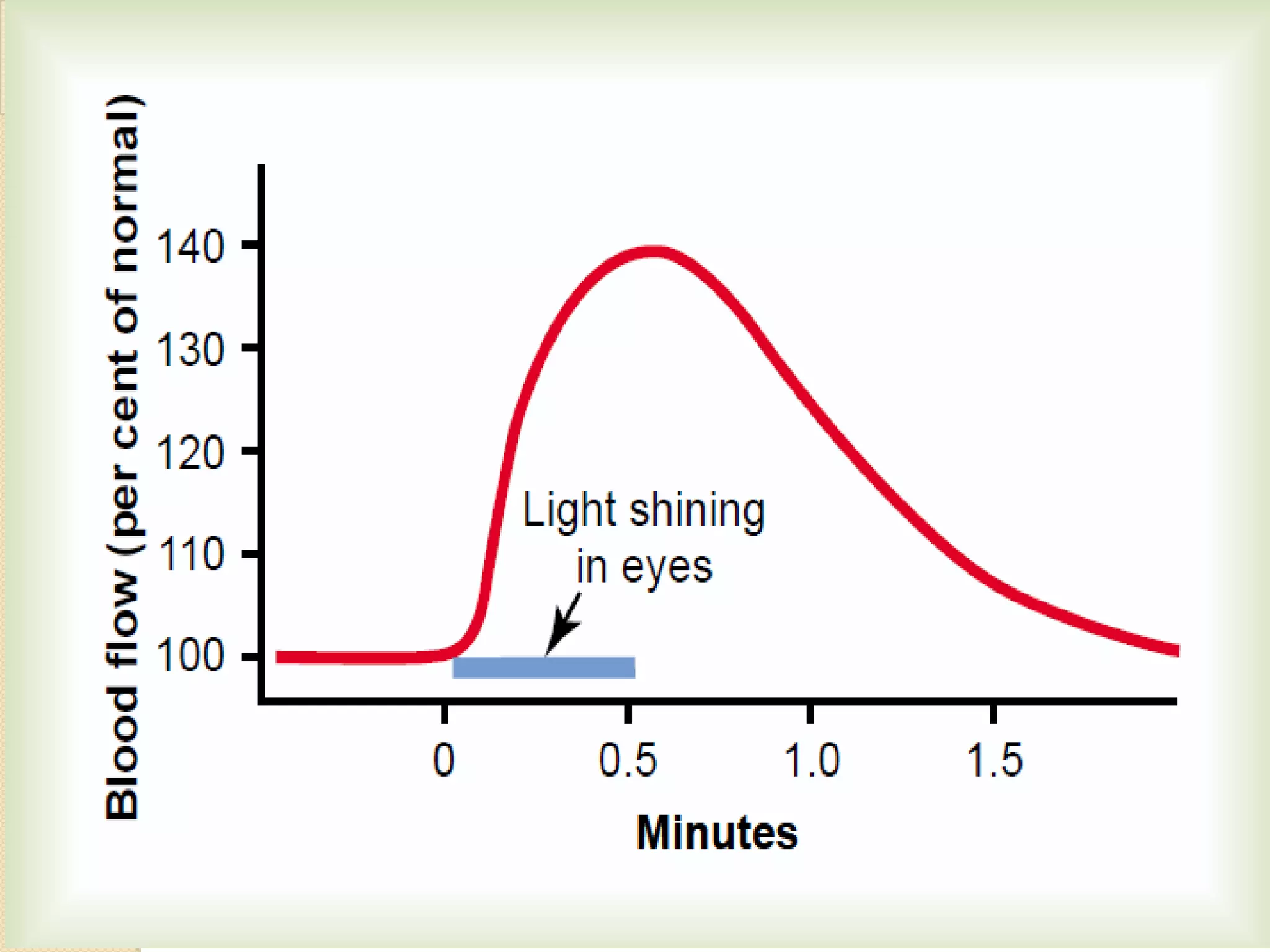
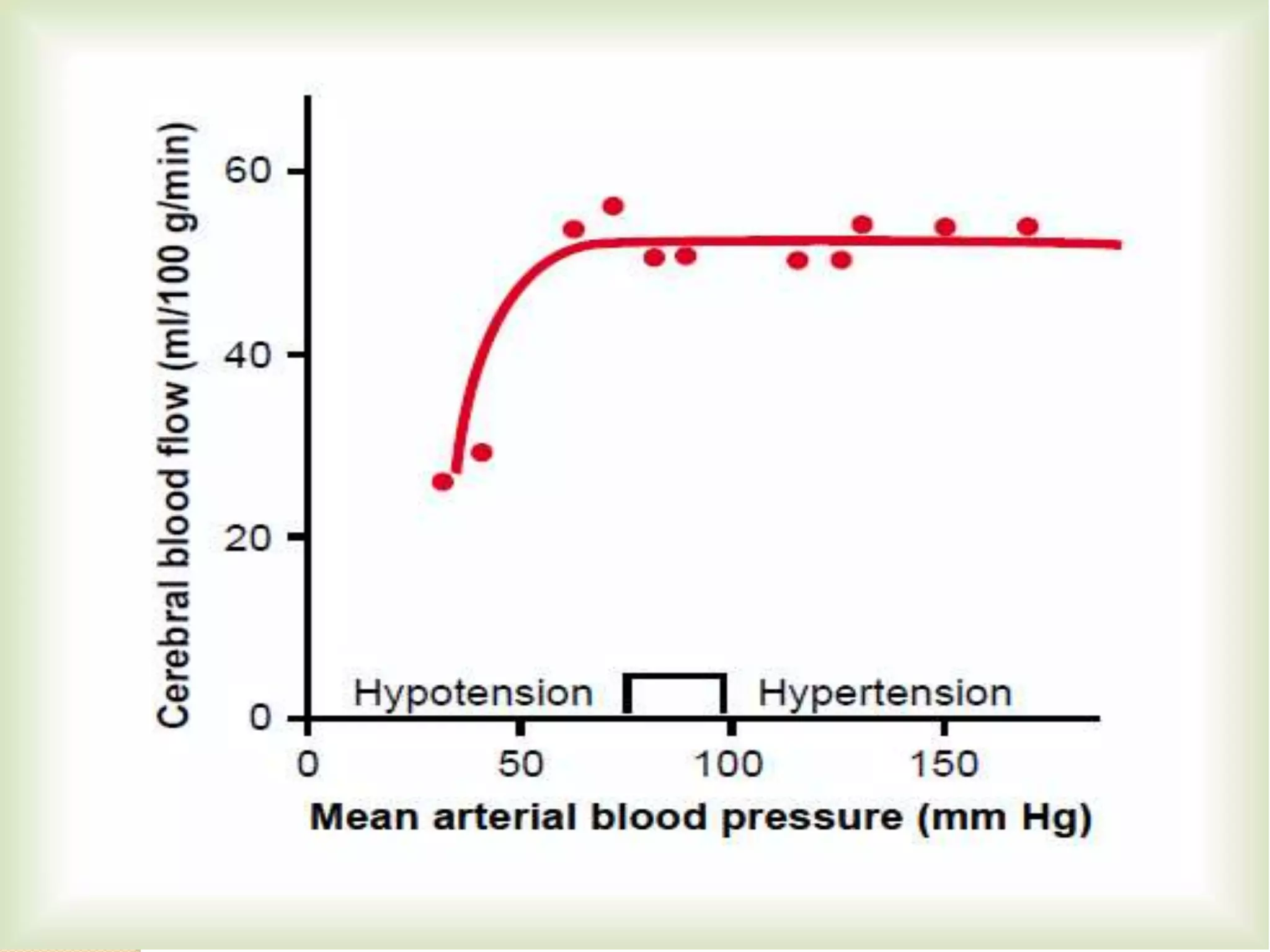
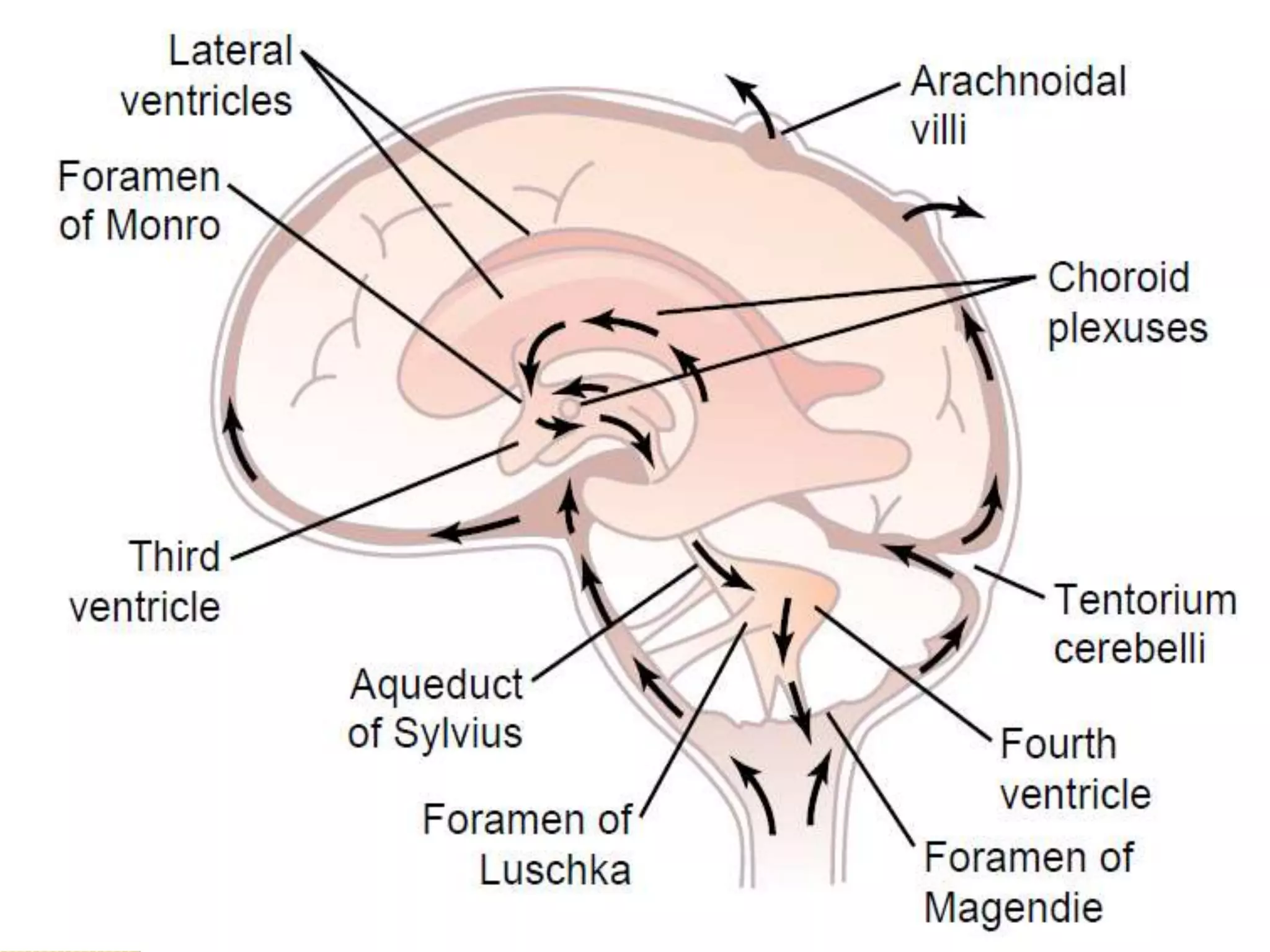
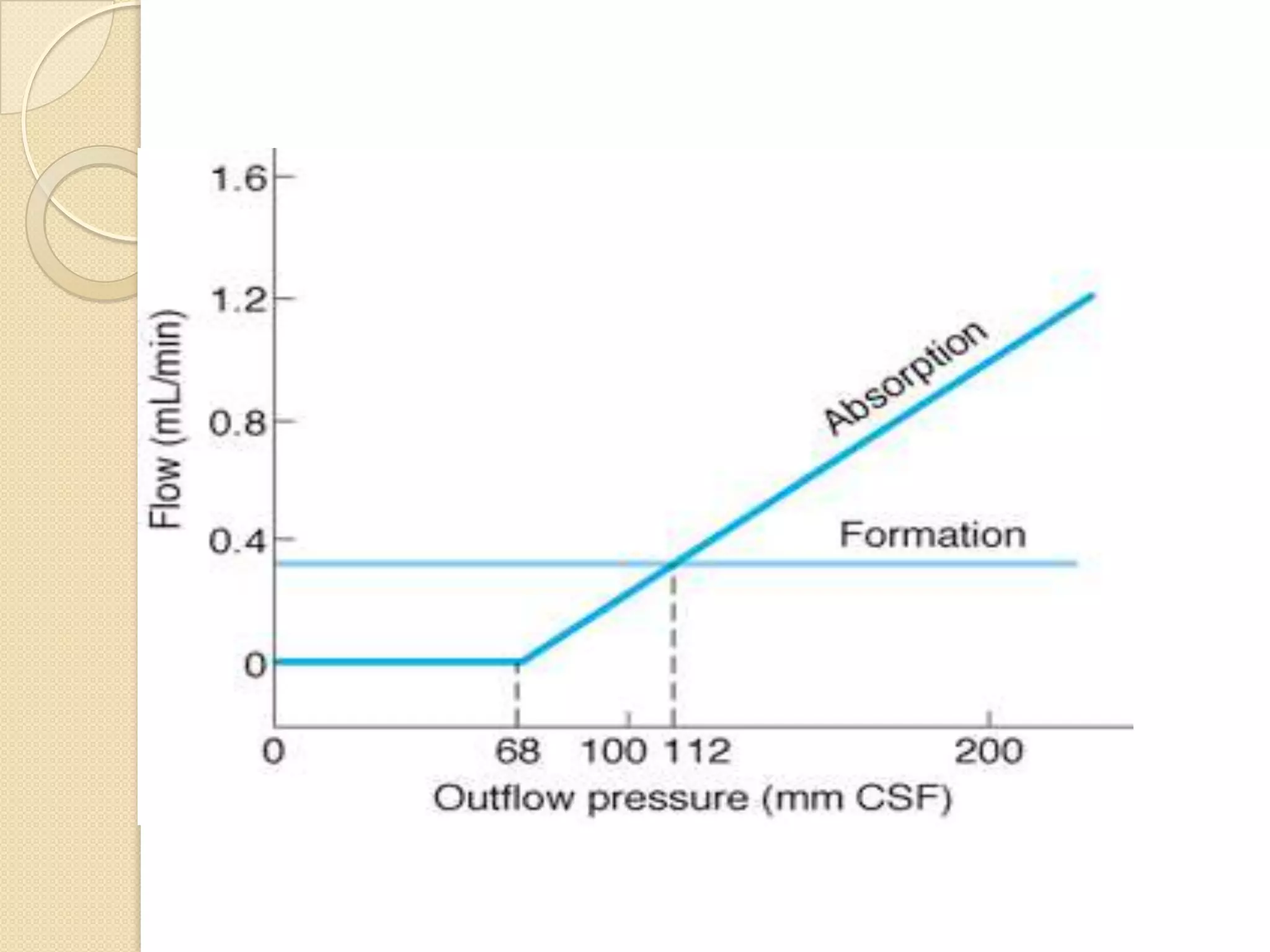
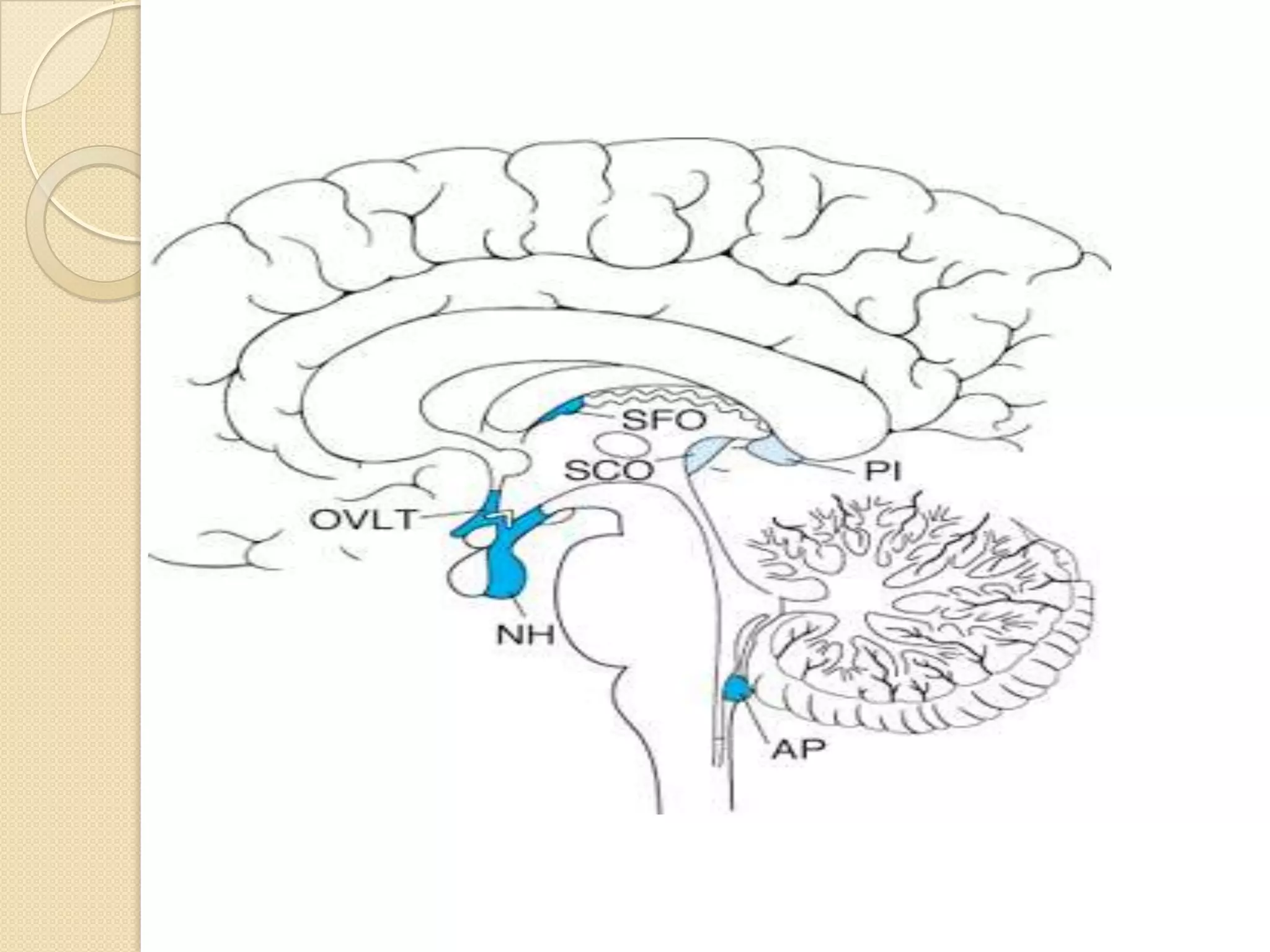
This document discusses cerebral circulation and factors that regulate cerebral blood flow. Three main factors control cerebral blood flow: carbon dioxide concentration, hydrogen ion concentration, and oxygen concentration. Increased carbon dioxide or hydrogen ions cause vasodilation and increased blood flow, while low oxygen triggers the oxygen deficiency mechanism to increase flow. Cerebral blood flow is also autoregulated between arterial pressures of 60-140 mmHg. The cerebrospinal fluid acts as a cushion for the brain and is circulated and absorbed via the choroid plexus and arachnoid villi. Increased cerebrospinal fluid pressure can cause papilledema and hydrocephalus. The blood-brain barrier tightly regulates molecular exchange between blood and brain tissue.