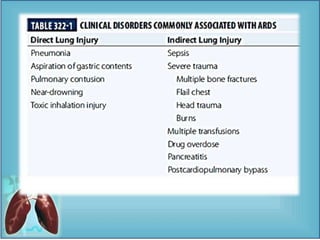
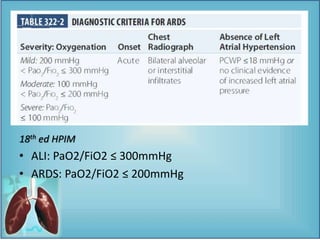
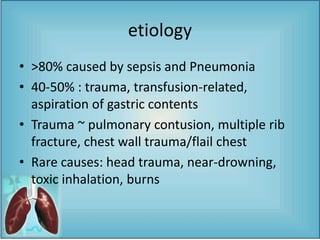
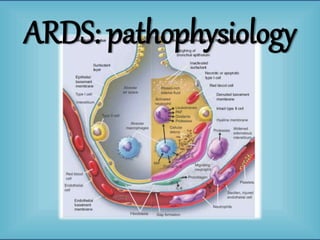
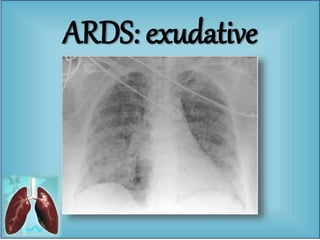
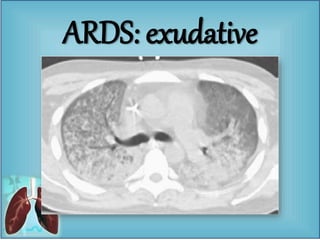
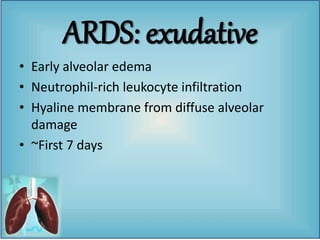
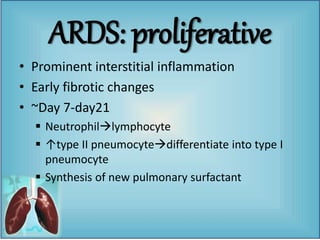
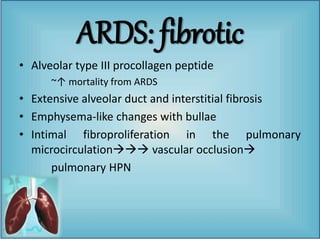
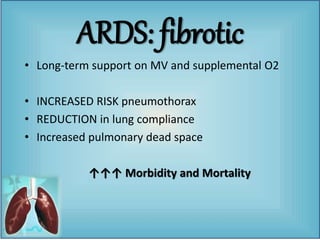
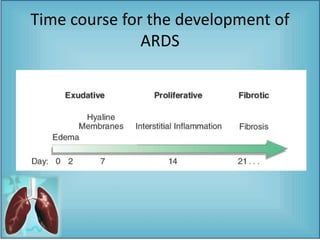
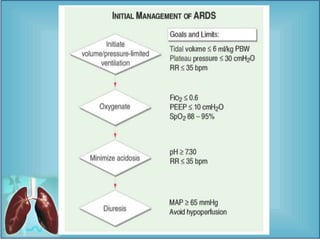
- Acute Respiratory Distress Syndrome (ARDS) is characterized by severe respiratory failure caused by diffuse lung injury from medical or surgical disorders. It involves three phases - exudative, proliferative, and fibrotic.
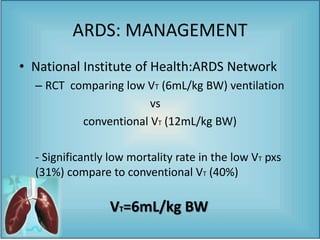
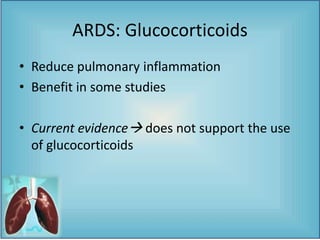
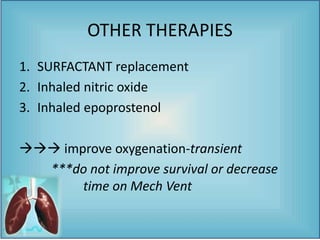
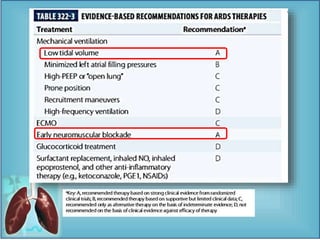
- The management of ARDS focuses on treating the underlying cause, lung-protective ventilation with low tidal volumes, use of PEEP to prevent alveolar collapse, and consideration of prone positioning. Adjunctive therapies like neuromuscular blockade and fluid restriction may help but other proposed therapies like steroids have not proven beneficial. Mortality remains high depending on severity of hypoxemia and presence of other organ failure.