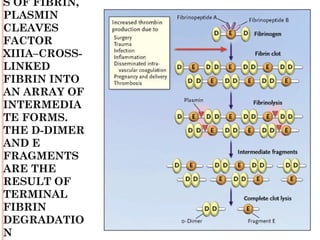
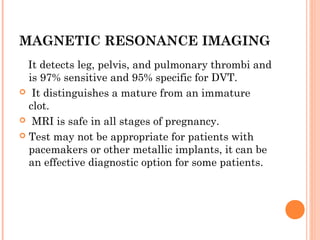
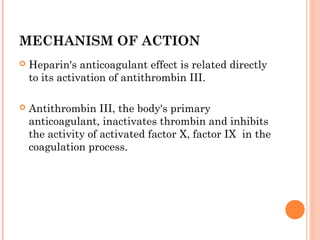
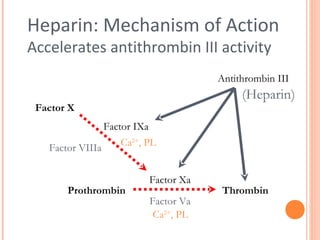
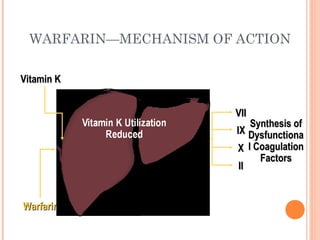
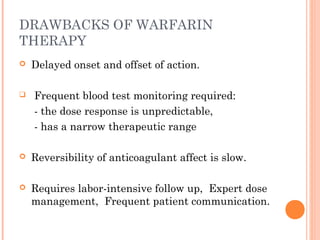
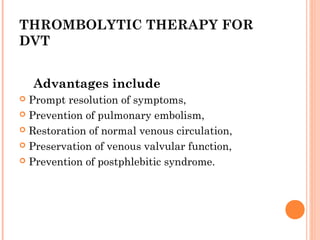
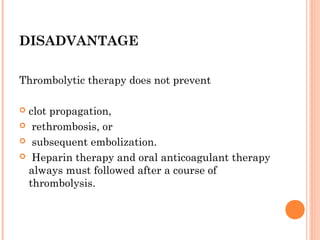
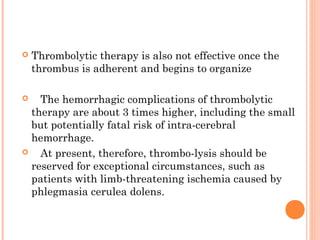
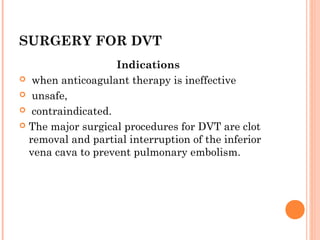
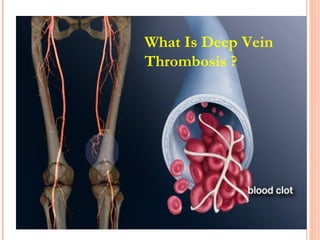
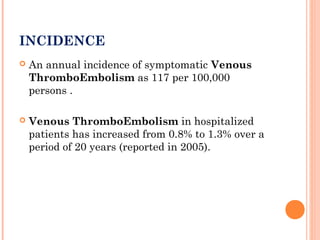
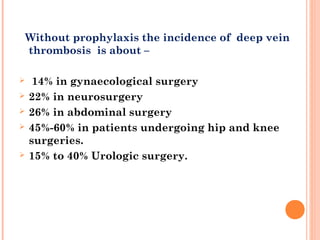
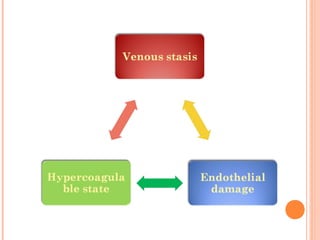
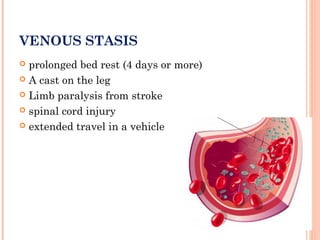
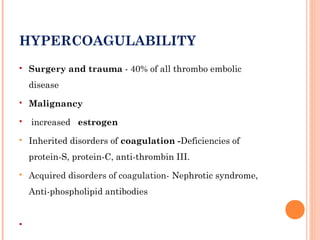
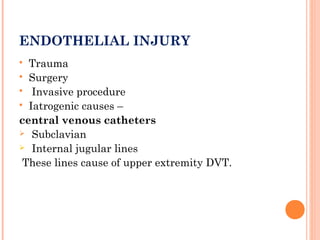
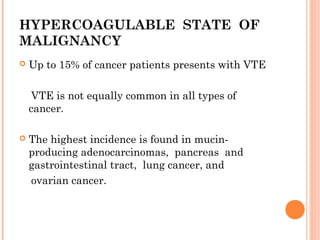
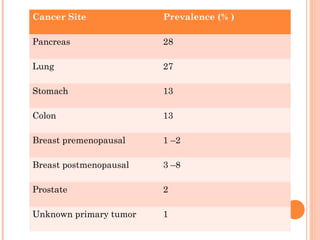
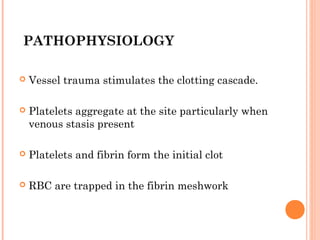
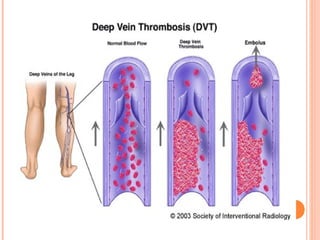
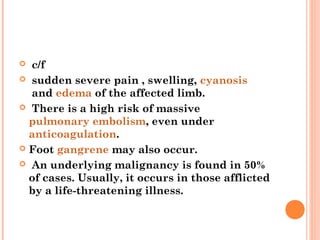
Deep vein thrombosis (DVT) is a blood clot that forms in the deep veins, usually of the legs. It can be asymptomatic or cause leg pain, swelling, warmth, and redness. Risk factors include prolonged bed rest, surgery, cancer, and inherited or acquired hypercoagulable states. Diagnosis involves the Wells criteria for pre-test probability followed by D-dimer testing and duplex ultrasound imaging of the legs. Treatment aims to prevent pulmonary embolism and includes bed rest, leg elevation, compression stockings, and anticoagulation medications like heparin or warfarin. Differential diagnoses include cellulitis, arthritis, and peripheral edema from other causes.

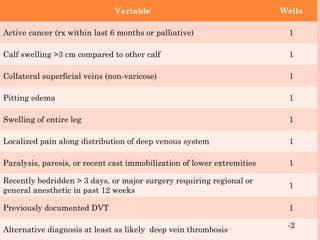
![Interpretation
High probability: ≥ 3 (Prevalence of DVT - 53%)
Moderate probability: 1-2 (Prevalence of DVT -
17%)
Low probability: ≤ 0 (Prevalence of DVT - 5%)
Adapted from Anand SS, et al. JAMA. 1998; 279
[14];1094](https://image.slidesharecdn.com/dvt-120917063342-phpapp02/85/Dvt-34-320.jpg)