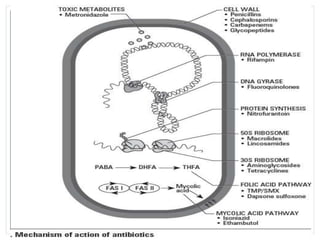
This document provides an overview of different classes of antibiotics, including cell wall inhibitors, protein synthesis inhibitors, topoisomerase inhibitors, anti-metabolites, and anti-mycobacterials. It describes common antibiotics within each class, what types of bacteria they cover, and examples of specific antibiotics. It also briefly discusses empiric antimicrobial therapy and treatment for C. difficile infections.















![Macrolides
[GP, Hemophilus, and atypical bacteria
(Legionella, Chlamydophila,
Mycoplasma)]
• erythromycin
• clarithromycin
• azithromycin](https://image.slidesharecdn.com/antibiotics-141028144224-conversion-gate01/85/Antibiotics-classification-and-spectrum-of-action-17-320.jpg)





















