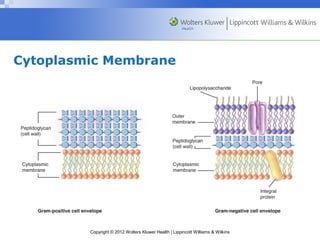
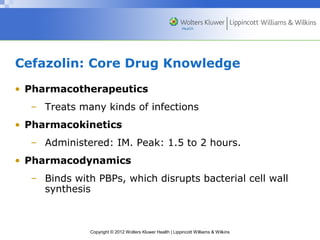
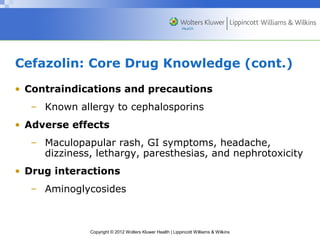
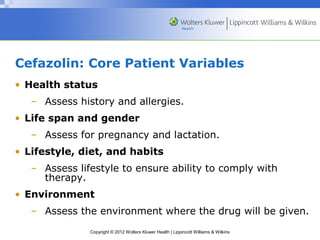
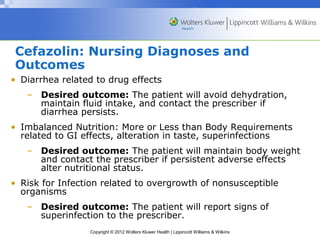
This document discusses several classes of antibiotics that affect the bacterial cell wall, including penicillins, cephalosporins, and vancomycin. It describes the mechanisms of action and molecular targets of these drugs and provides key information about their use, adverse effects, nursing considerations, and differences between generations or classes. The questions posed test understanding of administration routes for penicillin G and the effectiveness of first-generation cephalosporins against gram-negative bacteria.