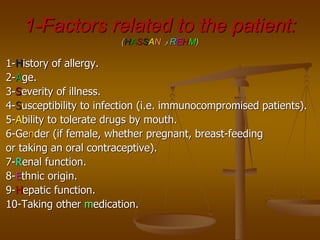
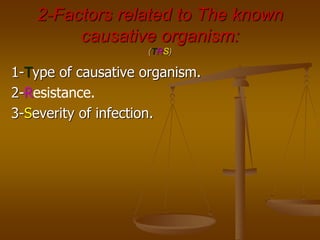
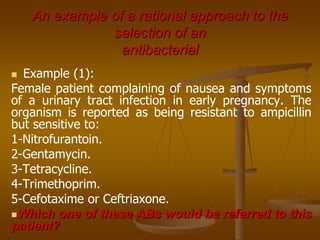
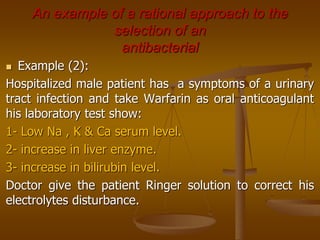
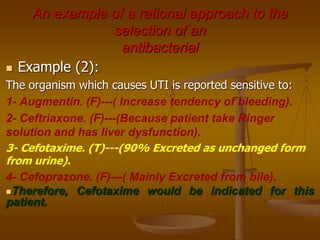
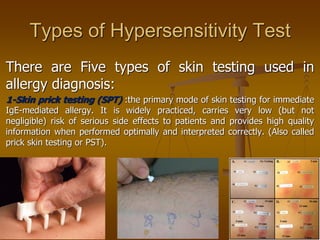
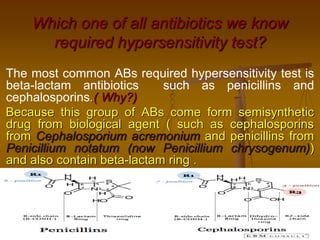
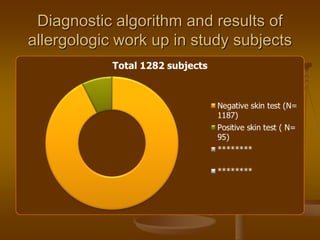
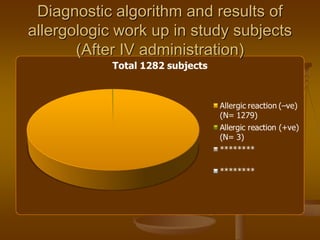
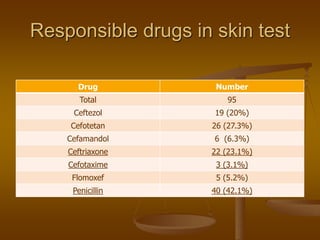
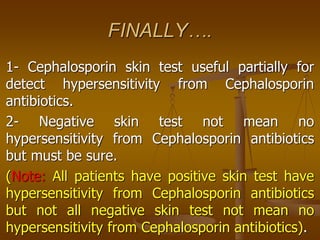
The document discusses strategies for selecting antibiotics based on patient factors and the causative organism. It provides examples of rational antibiotic selection for a pregnant woman with a UTI and a hospitalized man on warfarin taking antibiotics for a UTI. The document also discusses antibiotic policies, pre-treatment considerations like duration and route of administration, superinfections, and different types of hypersensitivity tests including skin prick, intradermal, and patch testing. It validates the use of cephalosporin skin testing to predict immediate hypersensitivity but notes negative tests do not rule out the possibility of hypersensitivity upon intravenous administration.