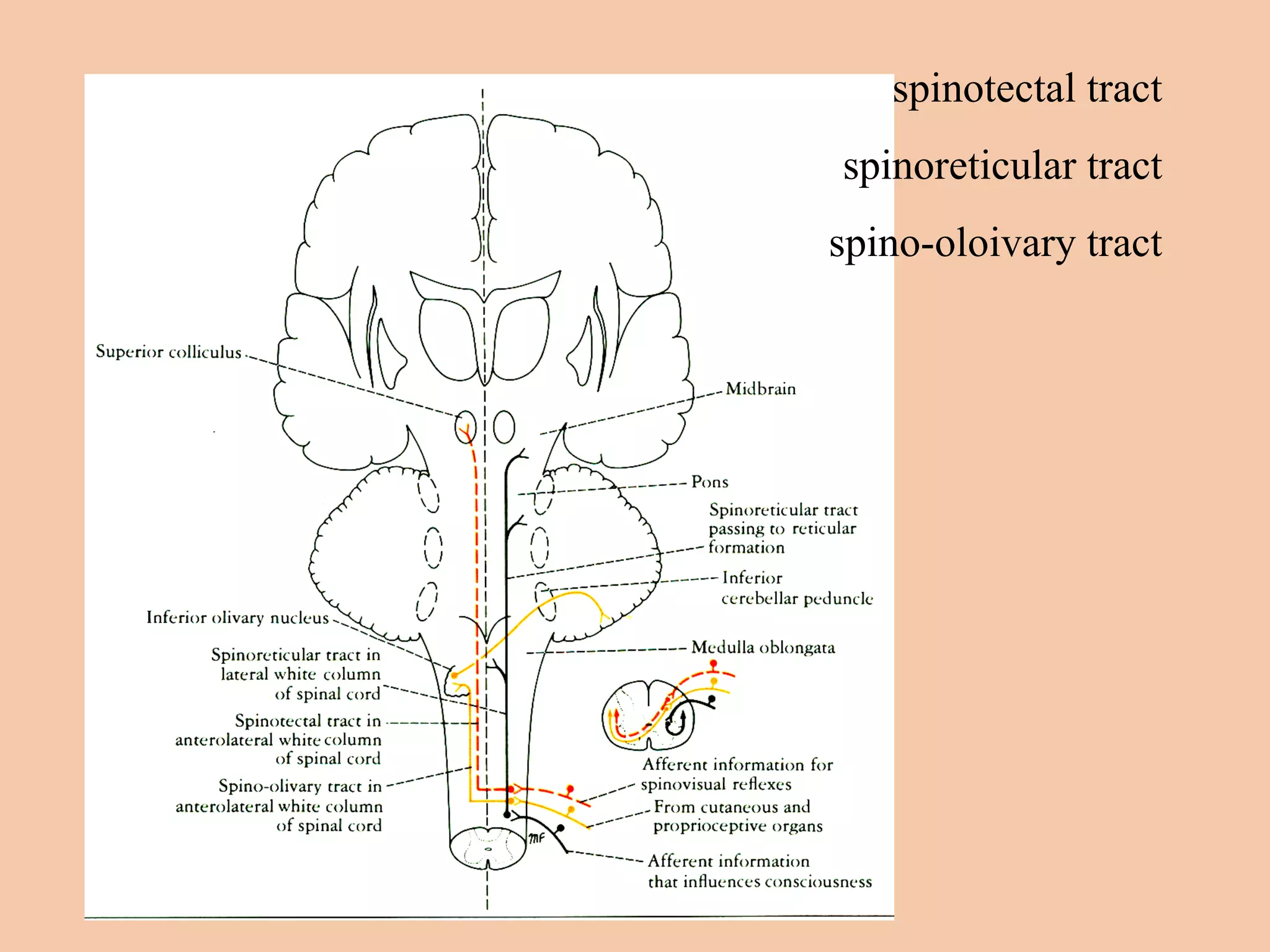
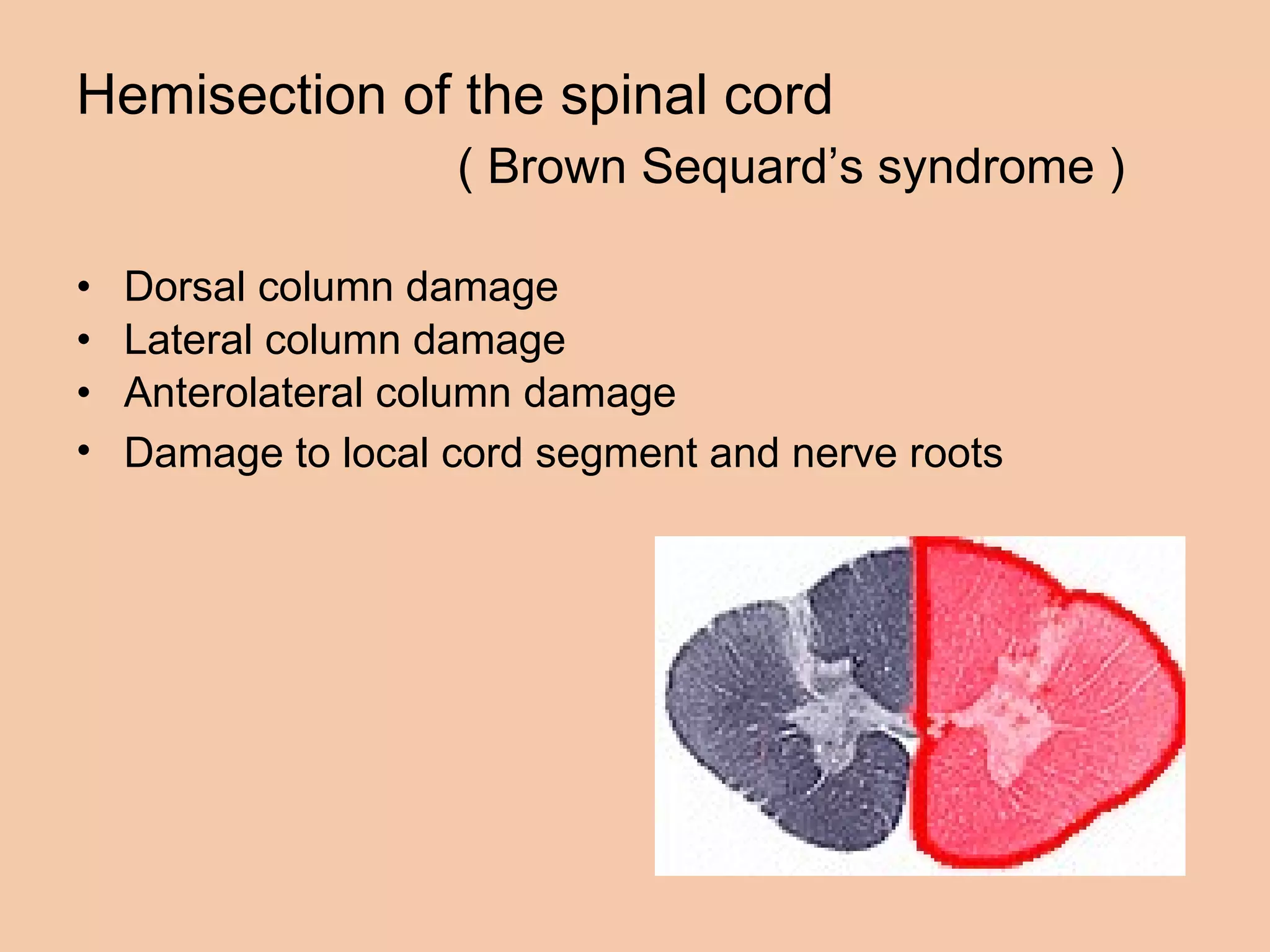
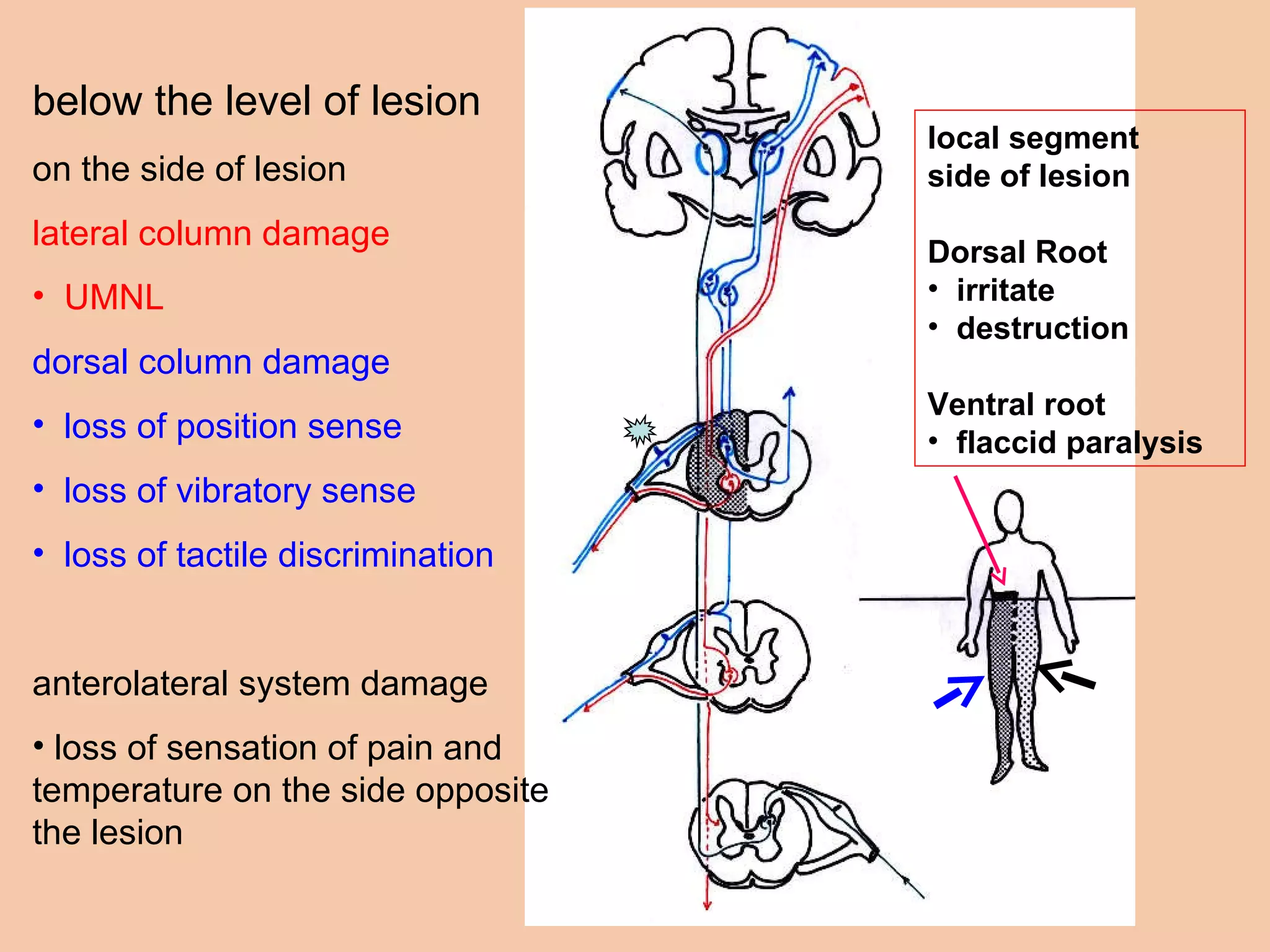
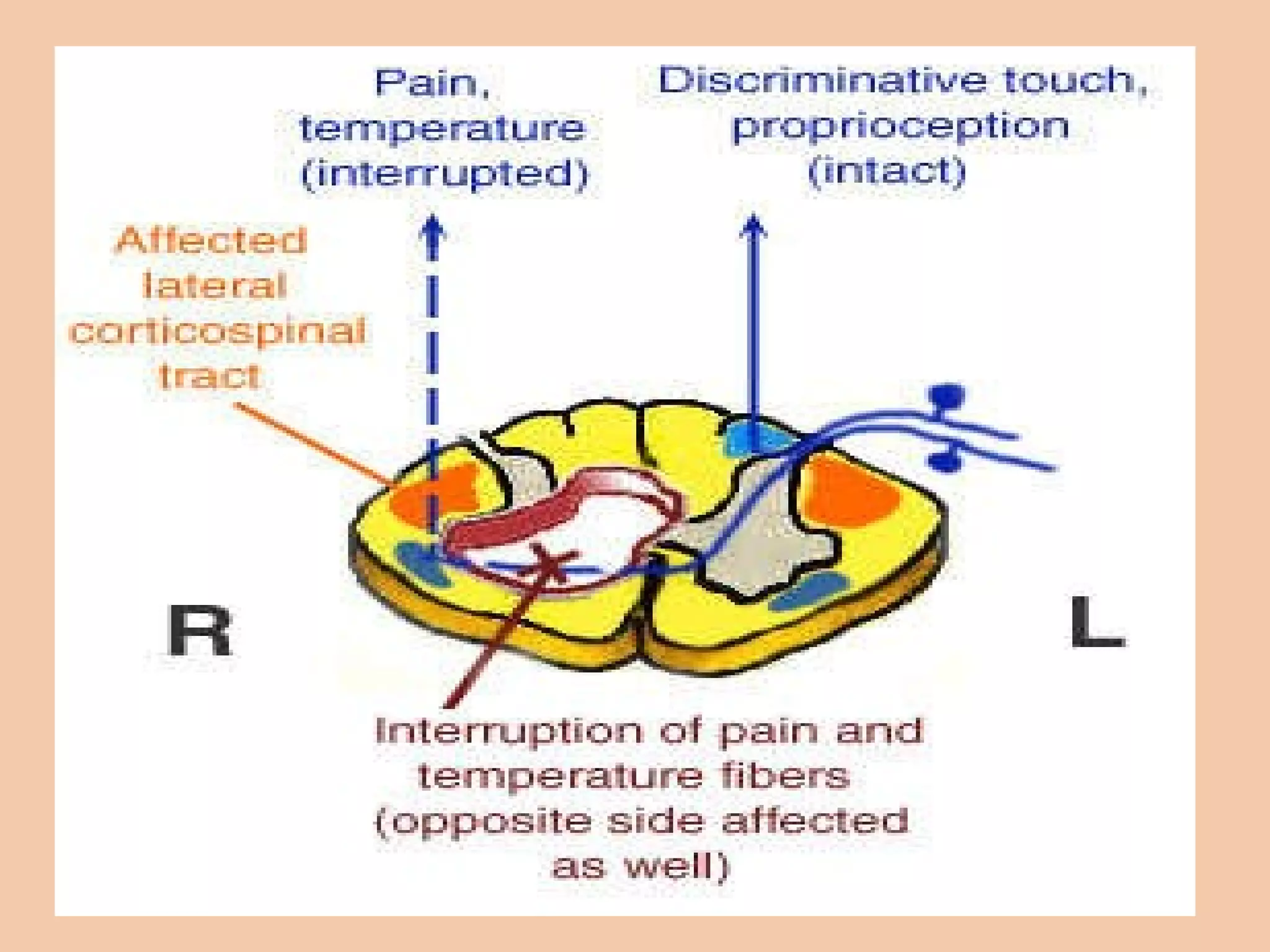
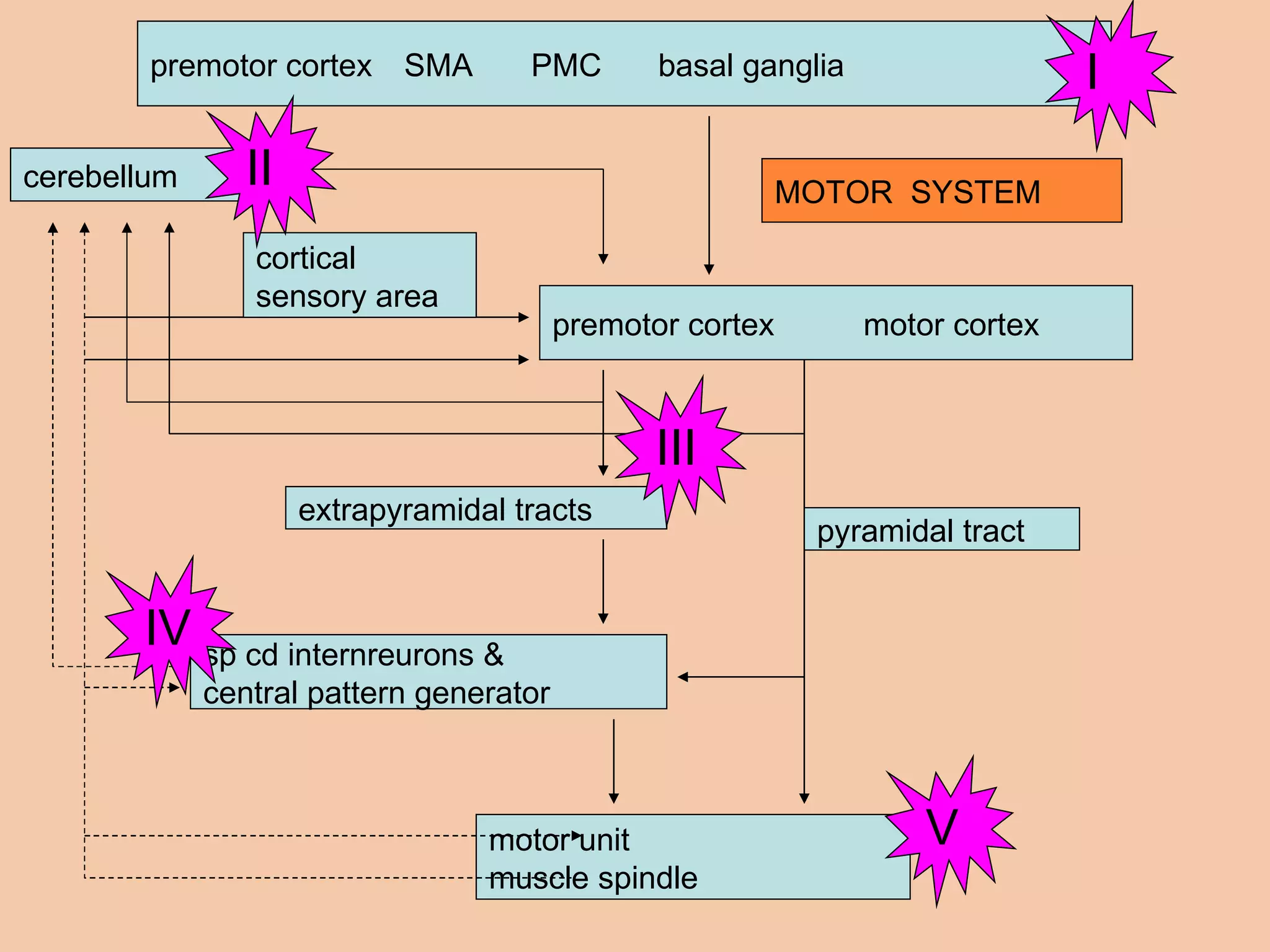
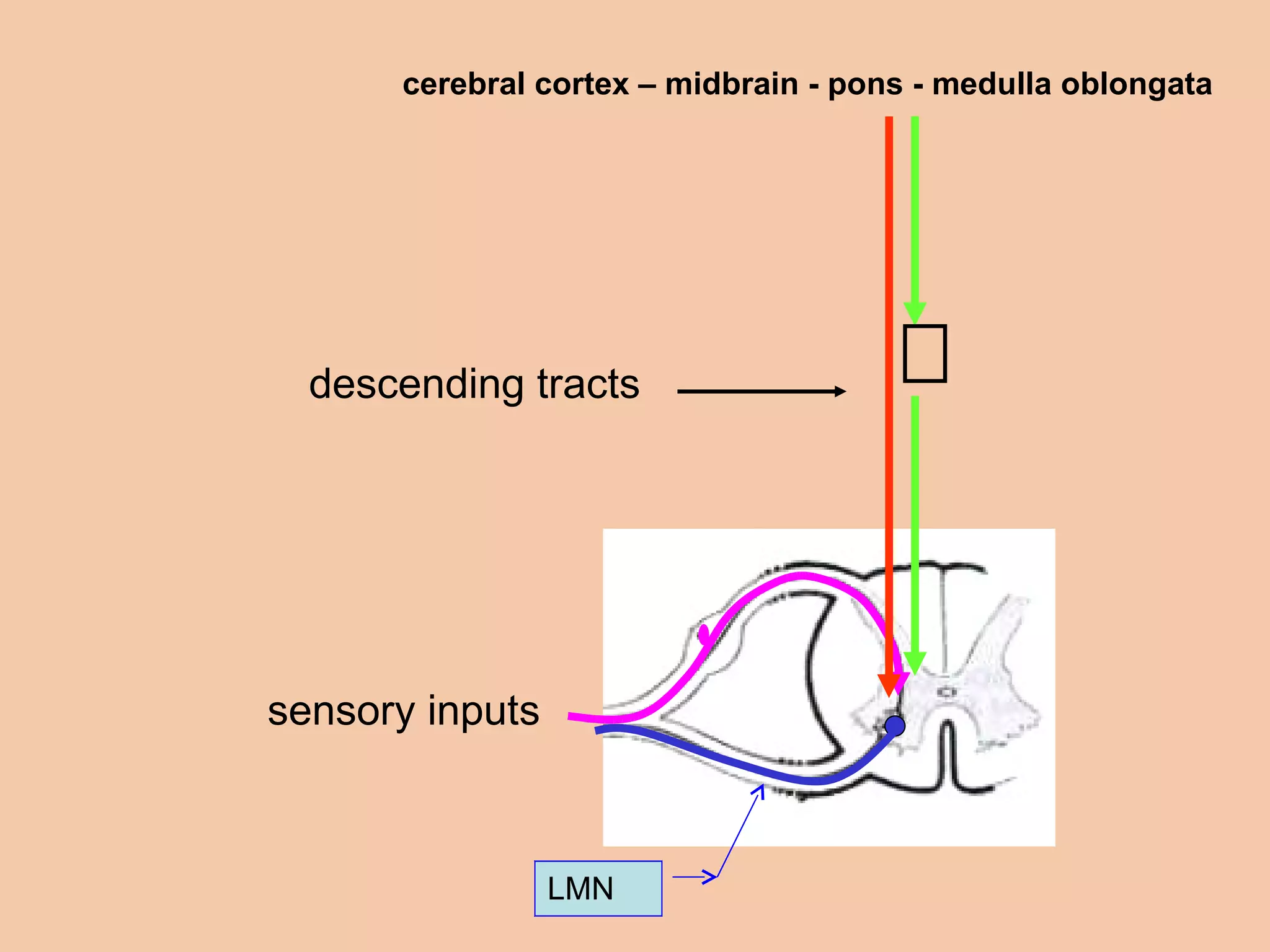
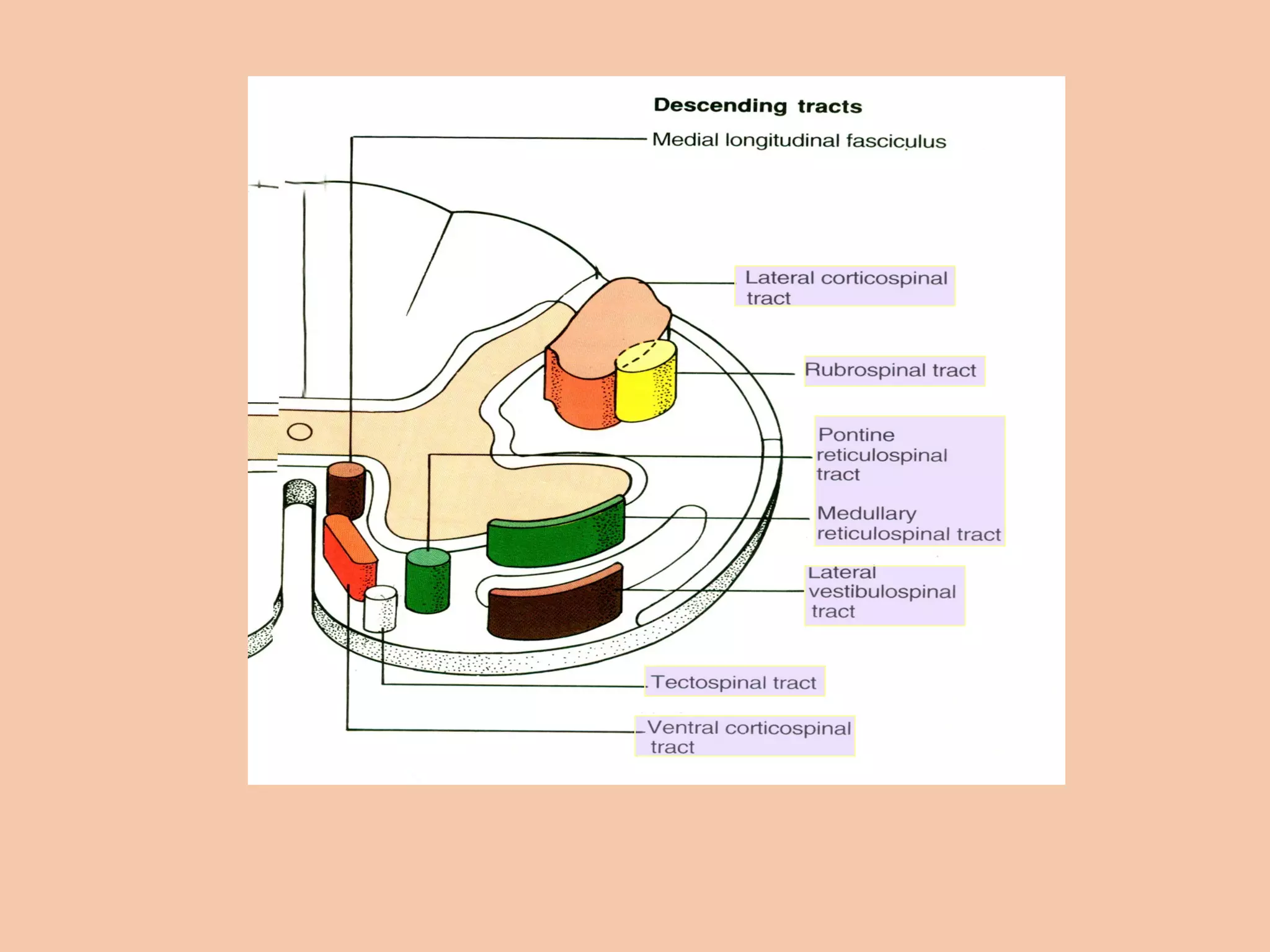
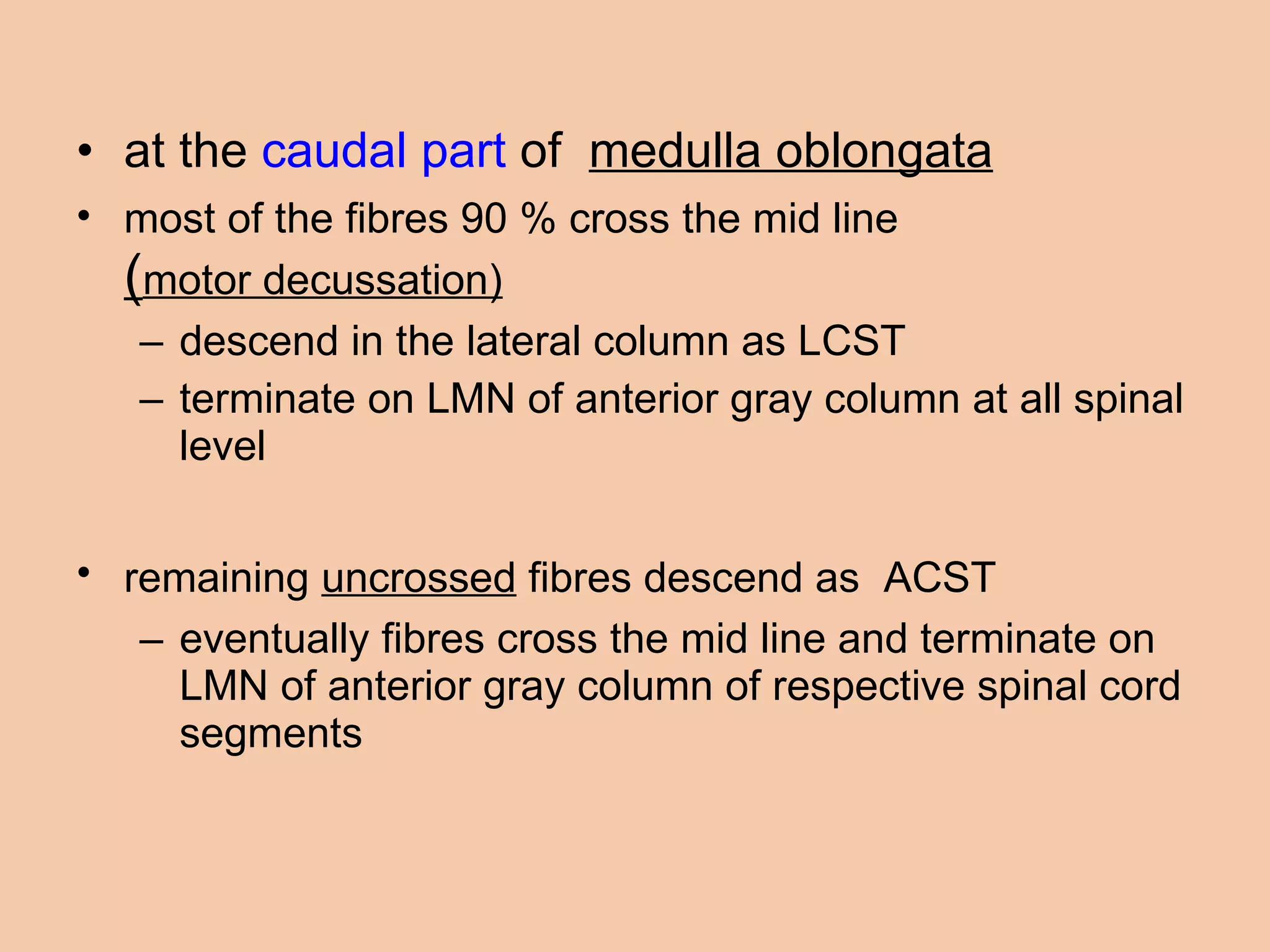
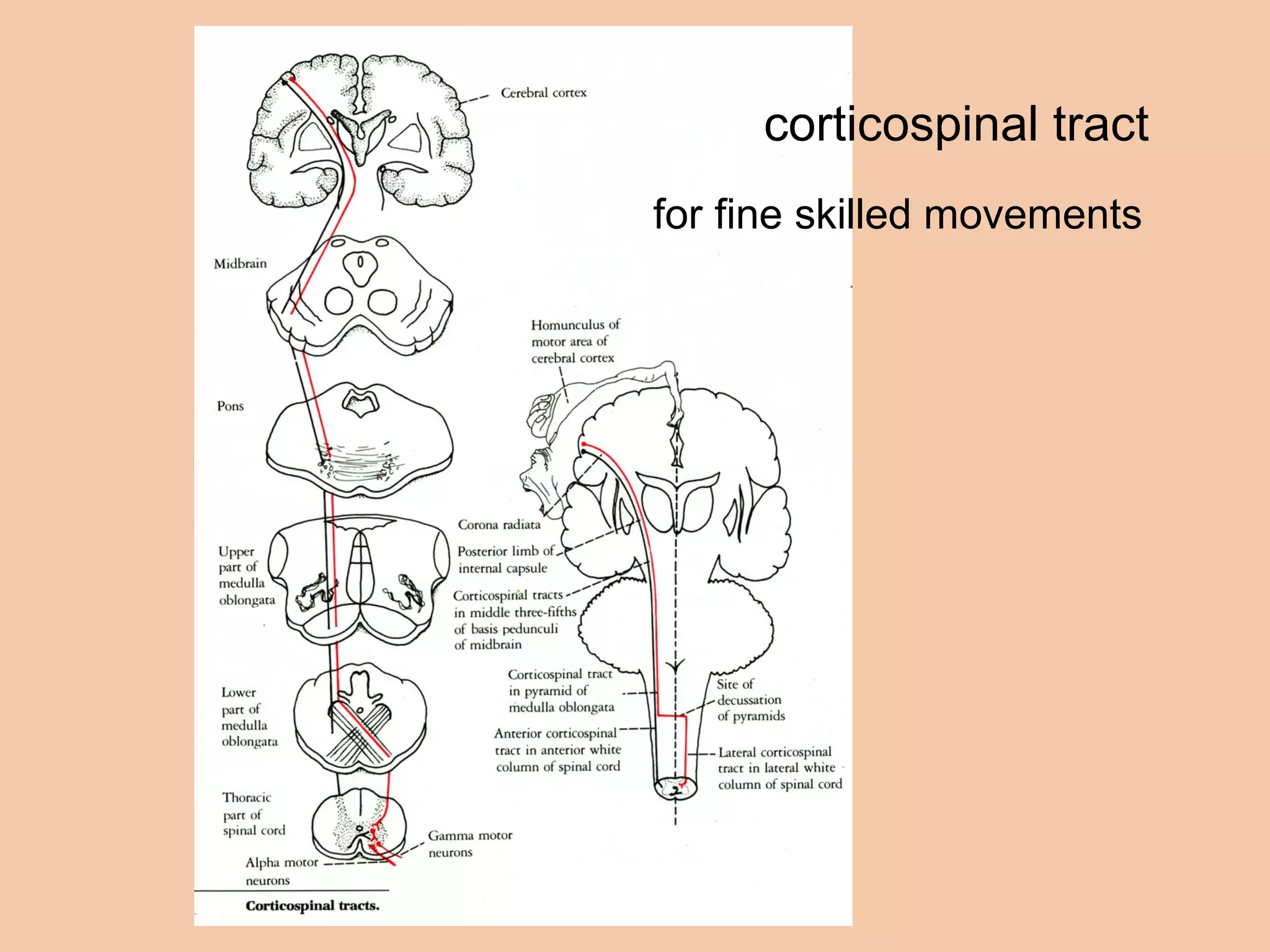
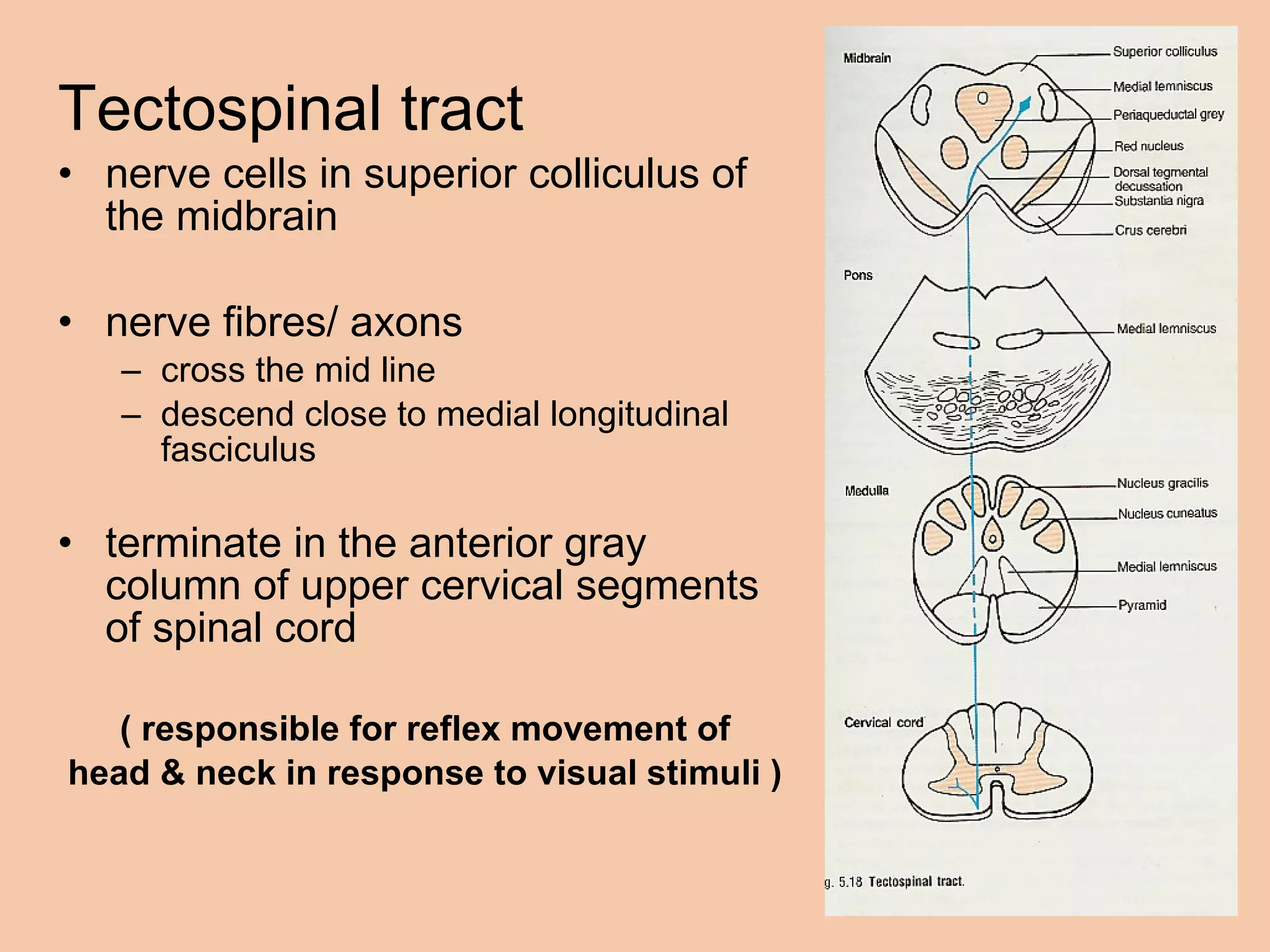
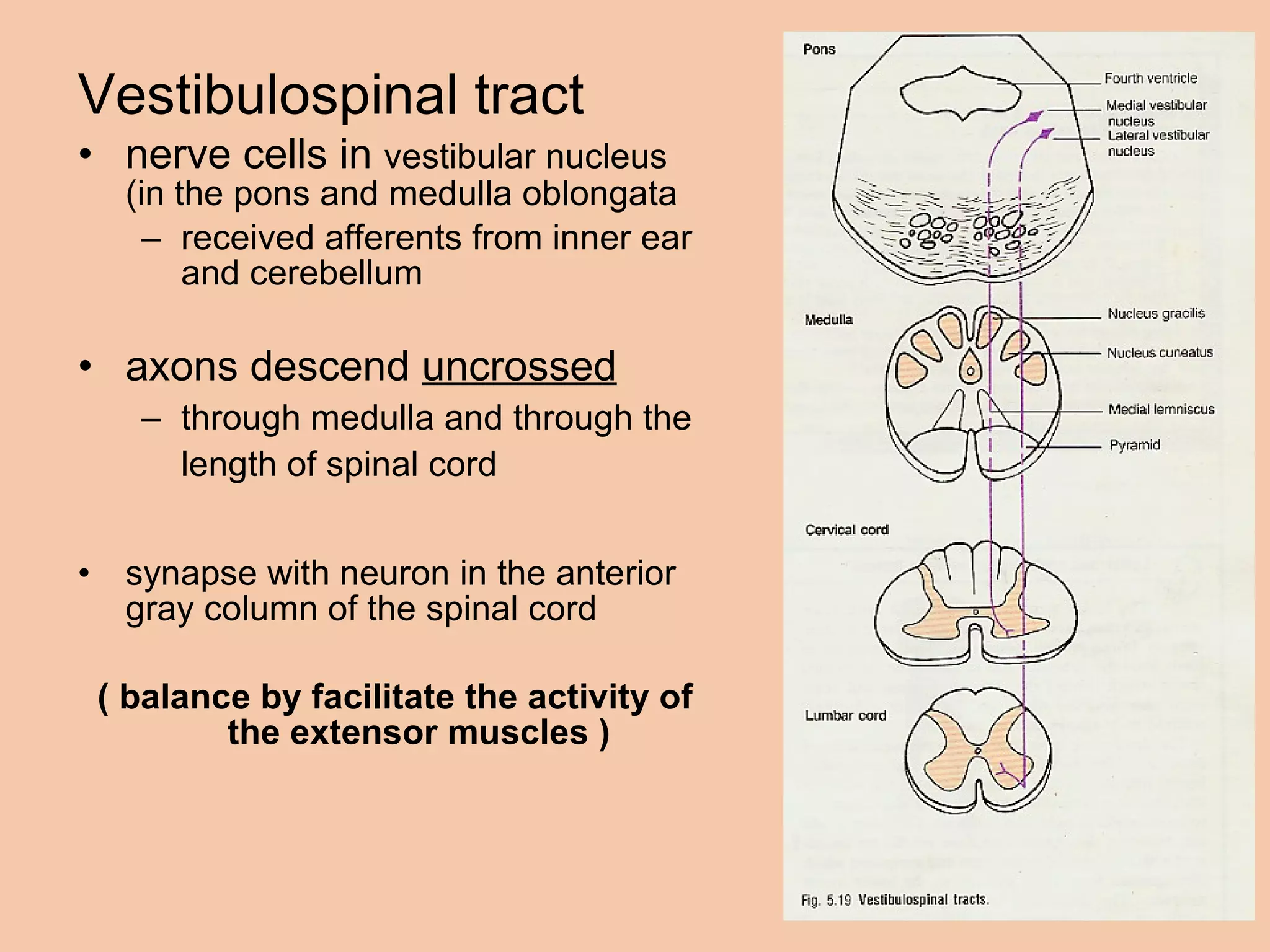
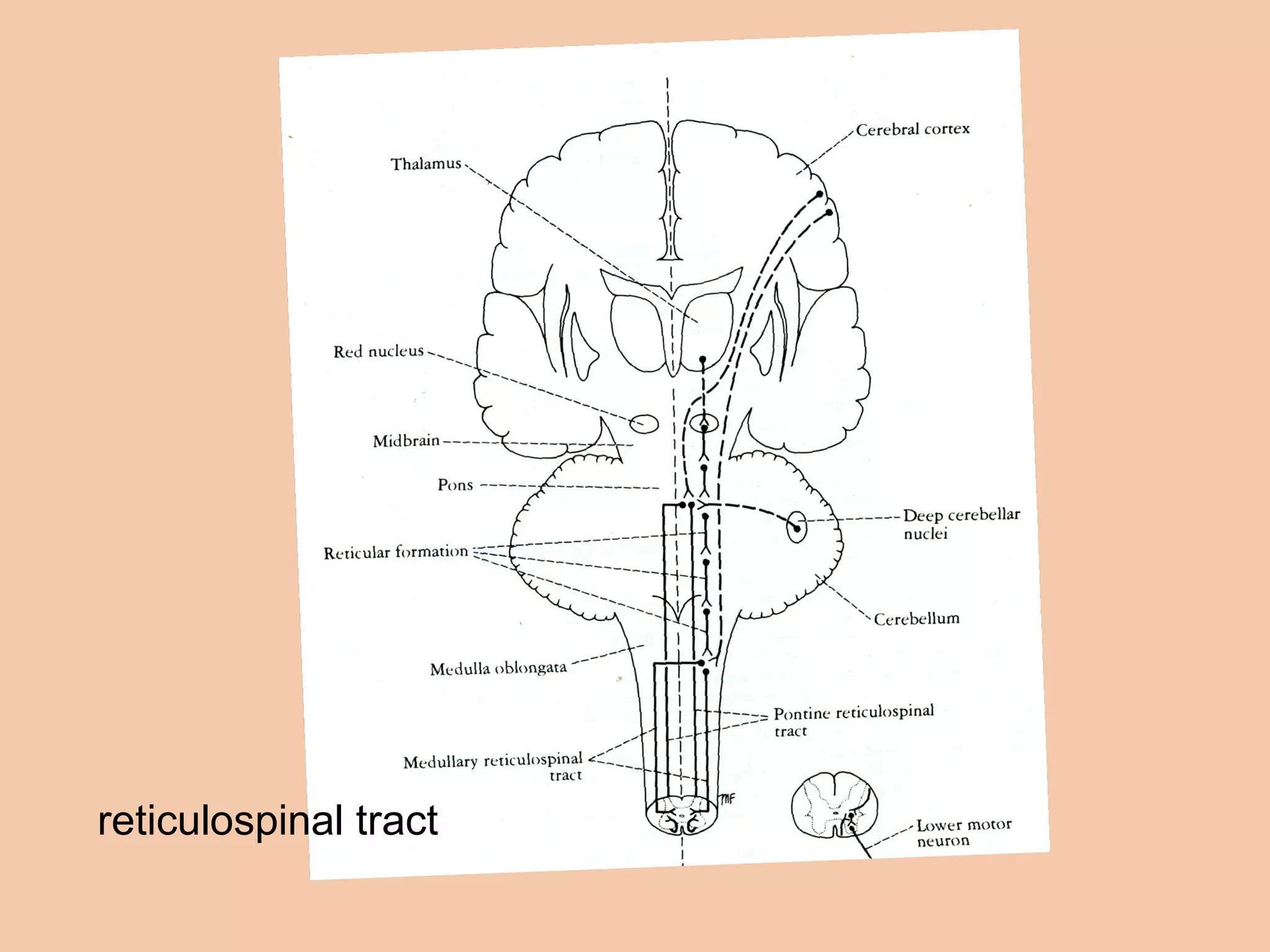
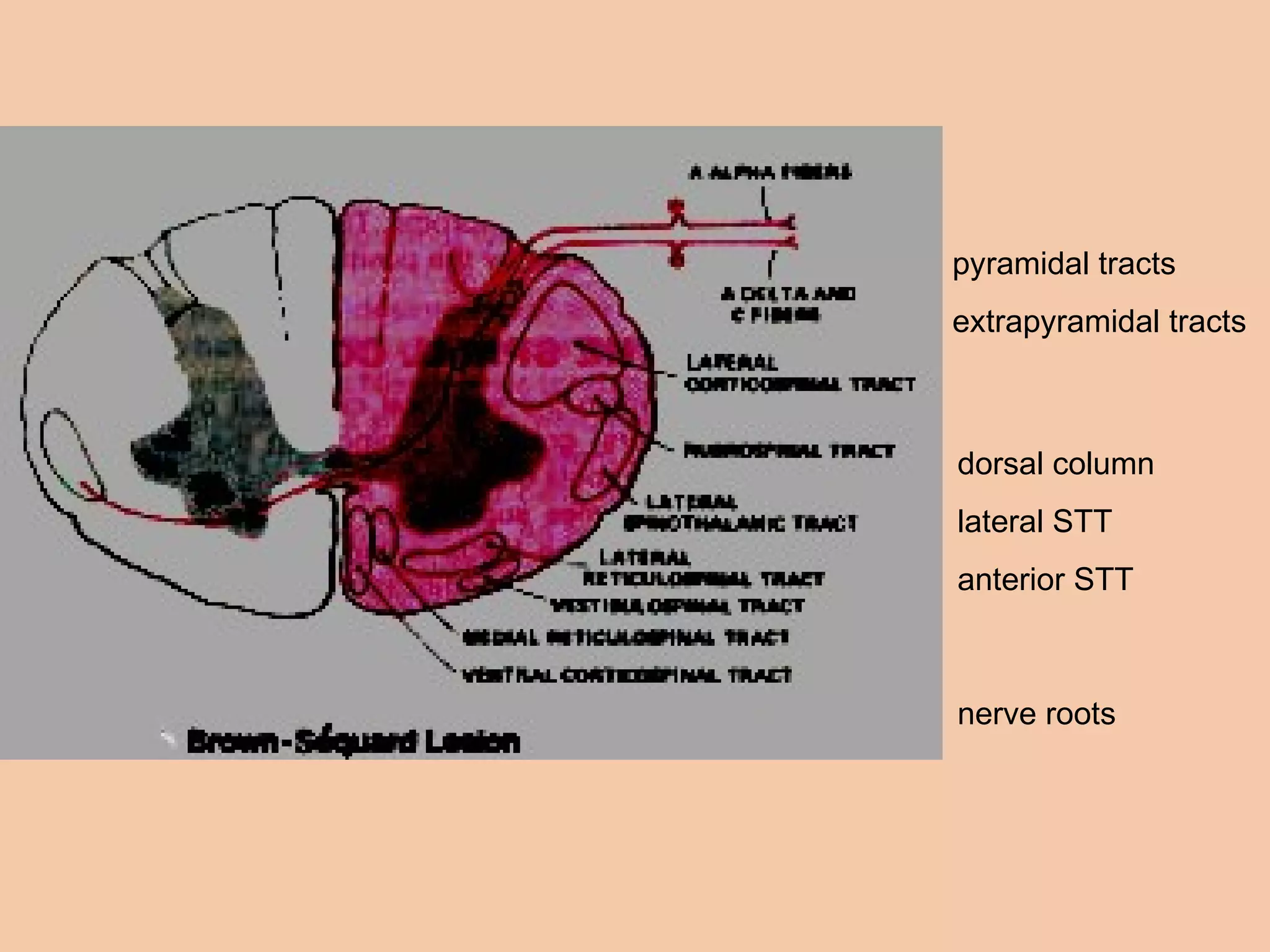
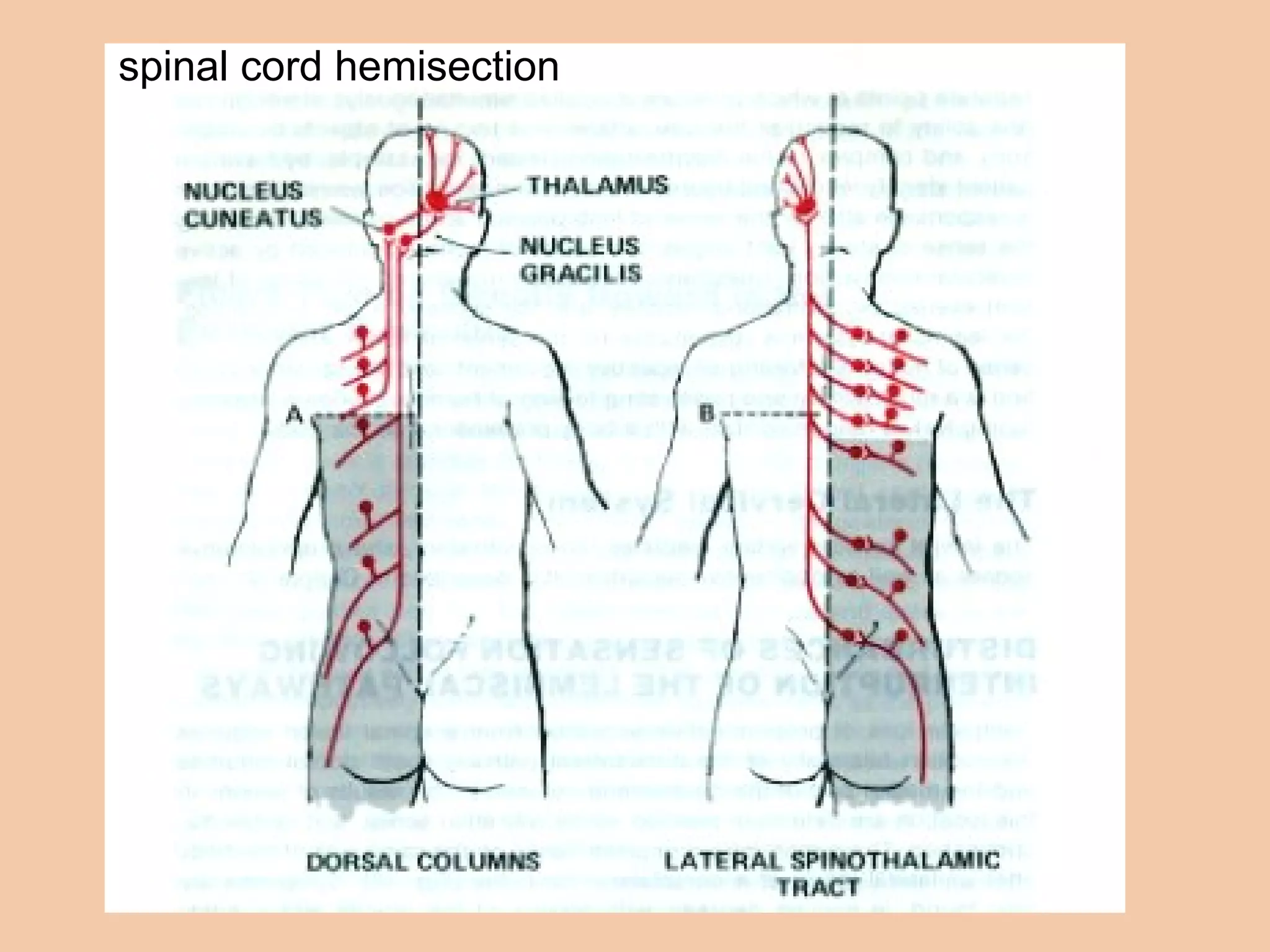
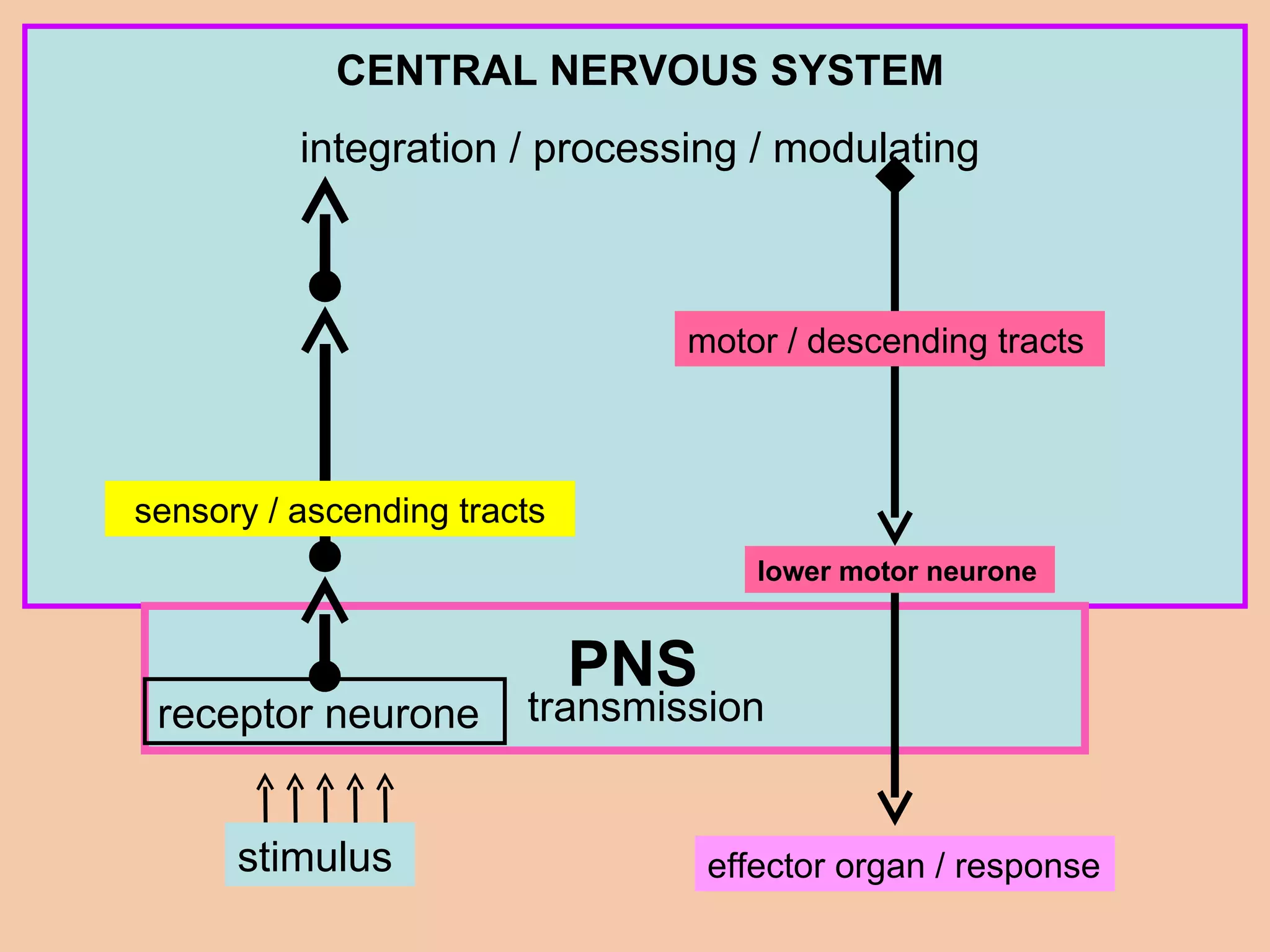
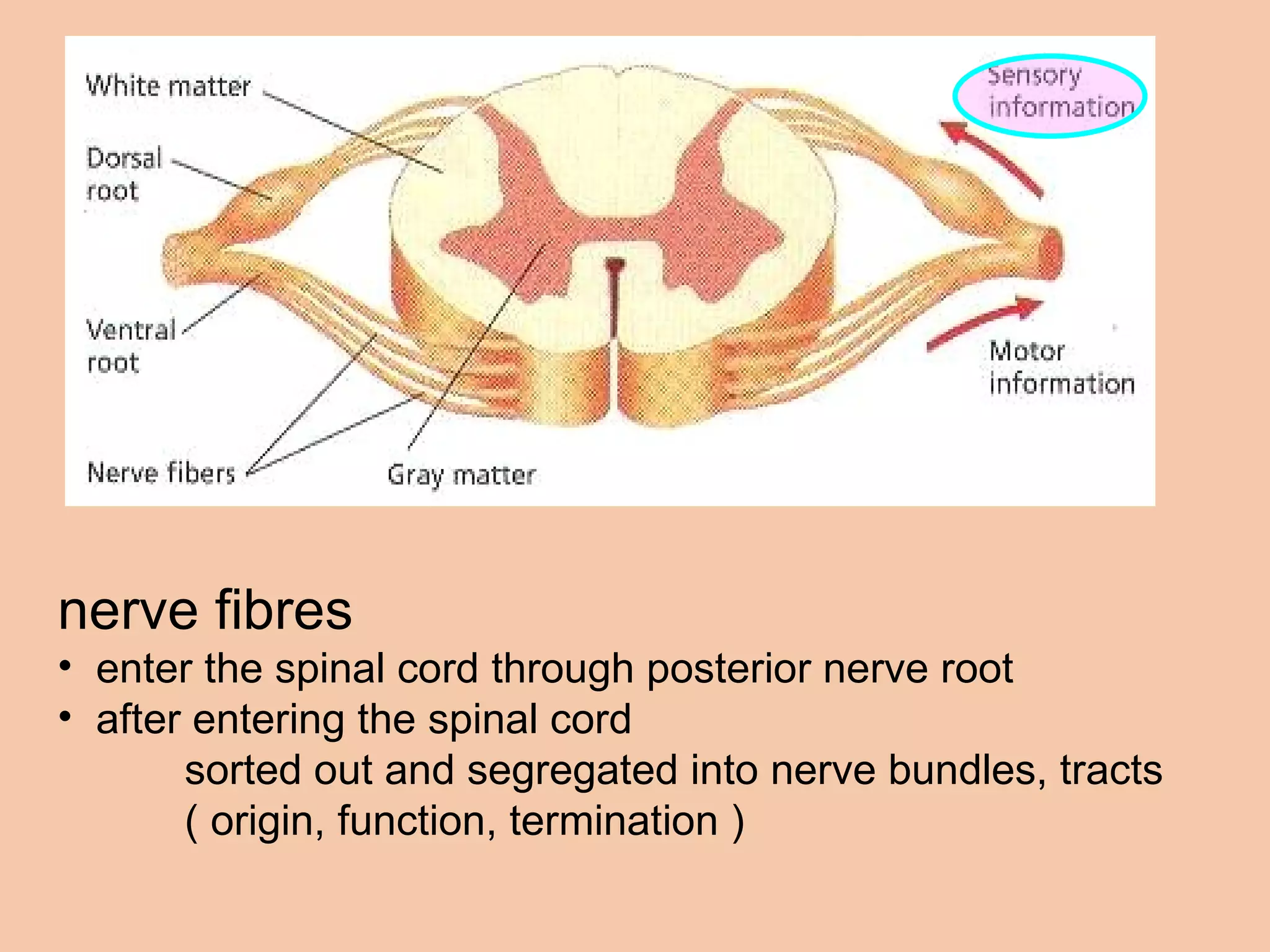
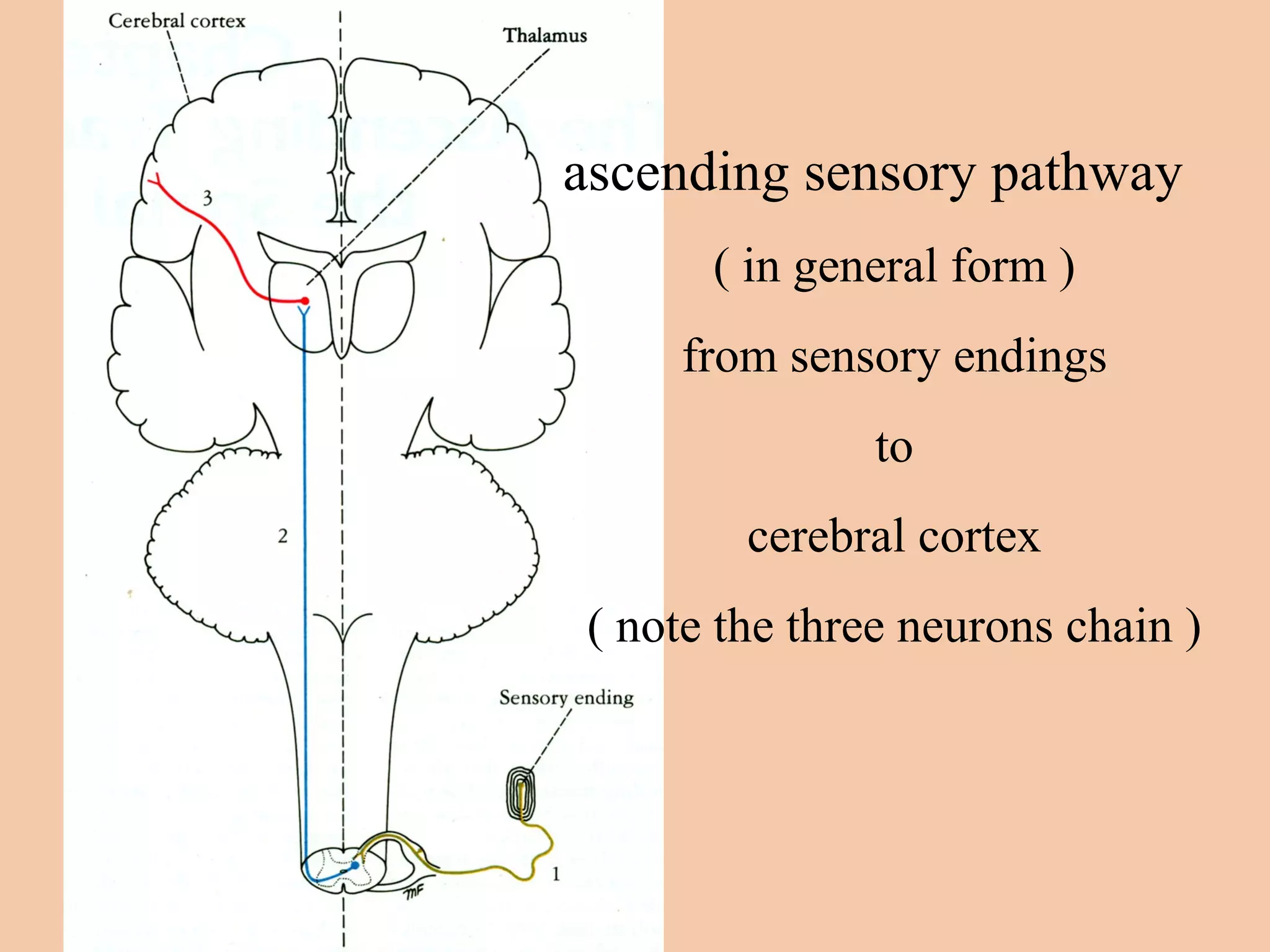
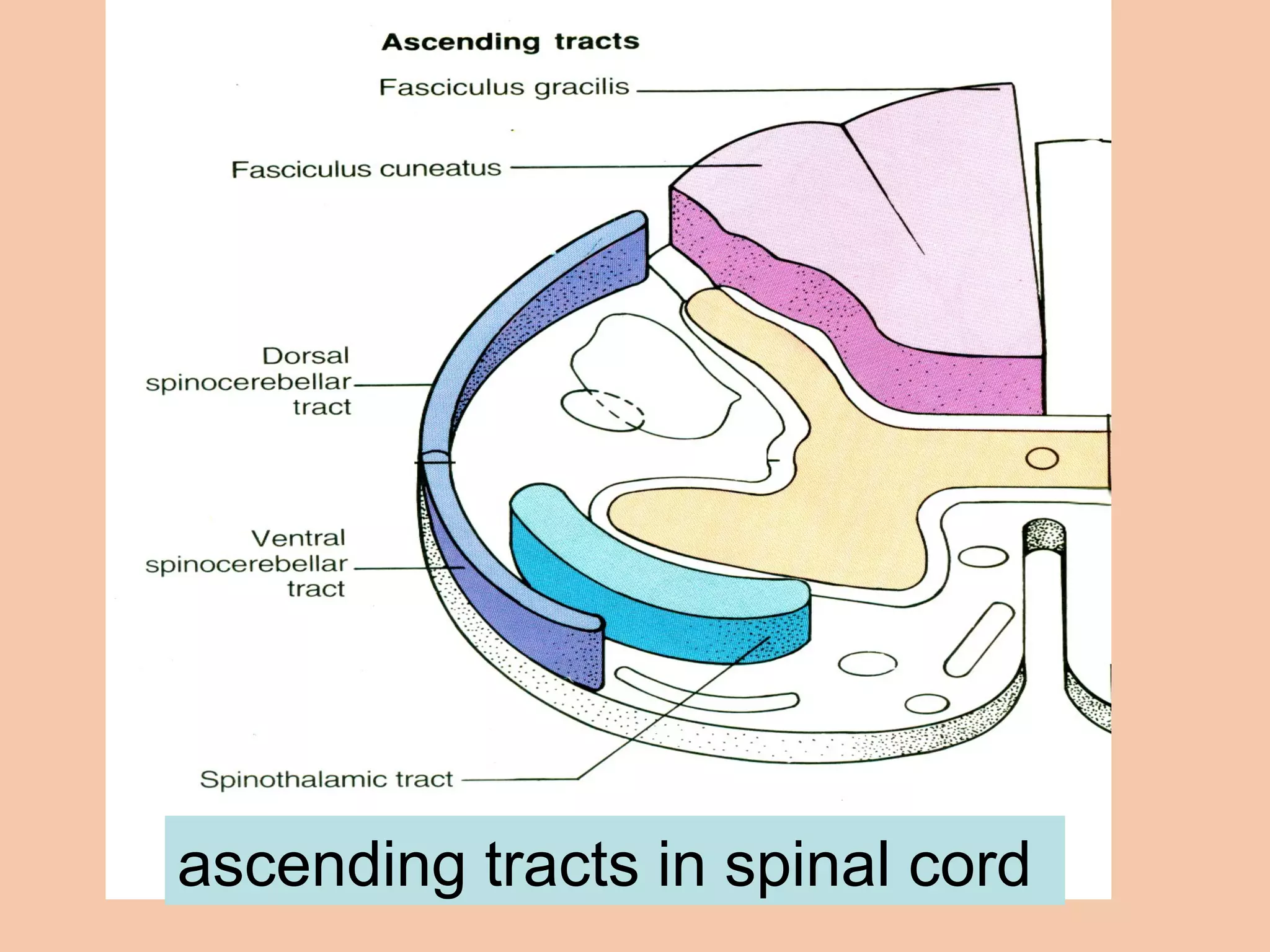
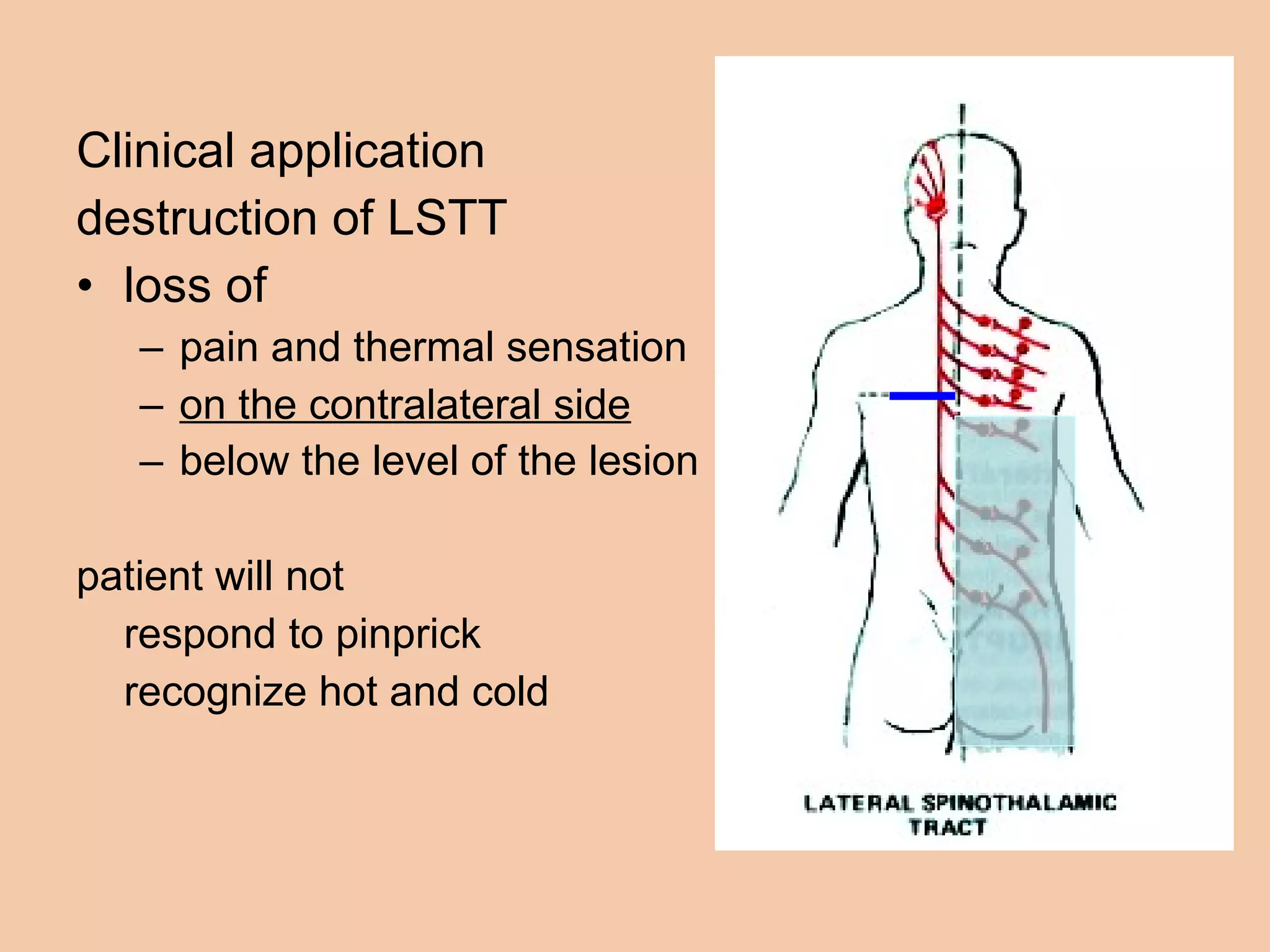
The document summarizes ascending and descending tracts in the spinal cord that transmit sensory and motor information between the spinal cord and brain. It describes the three neuron chain of ascending tracts that transmit exteroceptive, interoceptive, and proprioceptive sensory information from the peripheral receptors to the brain. It outlines the major ascending tracts - lateral and anterior spinothalamic tracts for pain/temperature and touch/pressure, and the posterior white column and cuneate and gracilis fasciculi for proprioception. It also summarizes the descending motor tracts including the corticospinal, rubrospinal, vestibulospinal, reticulospinal and tectospinal tracts that





















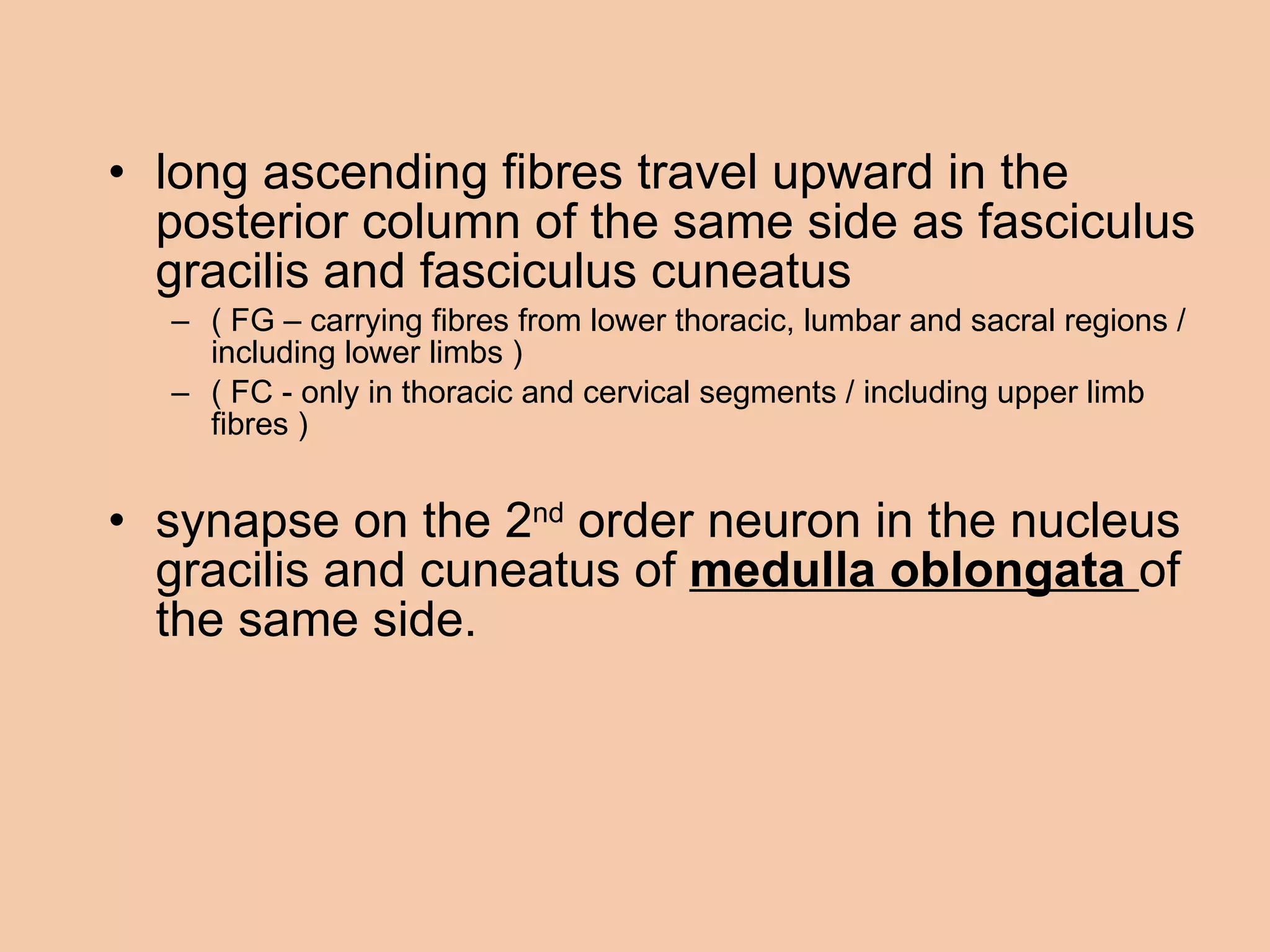
![lower 6 thoracic segments lumbar segments sacral segments cervical segments upper 6 thoracic segments fasciculus gracilis fasciculus cuneatus [ nucleus G & C ] in medulla G C](https://image.slidesharecdn.com/anatomyofascendinganddescendingtracts-100630161722-phpapp01/75/Anatomy-of-ascending-and-descending-tracts-37-2048.jpg)