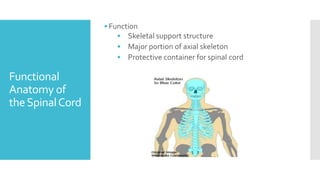
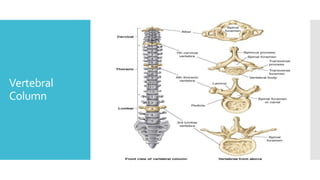
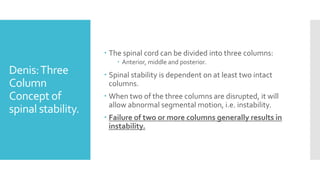
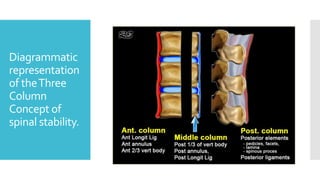
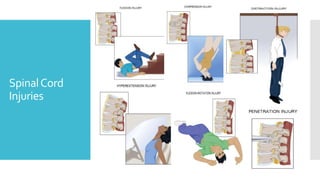
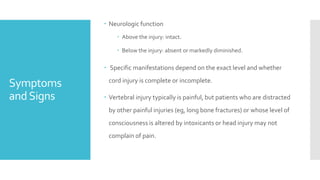
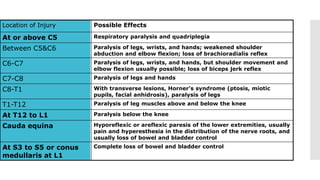
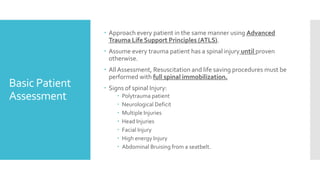
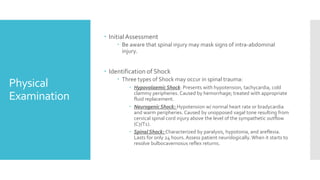
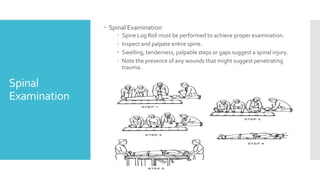
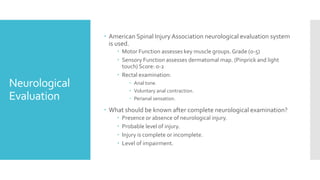
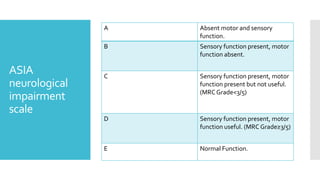
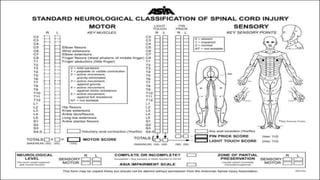
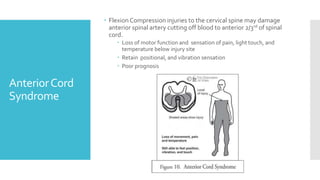
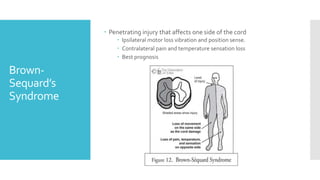
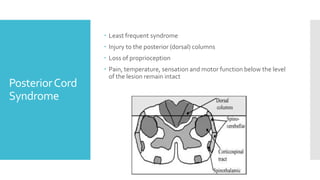
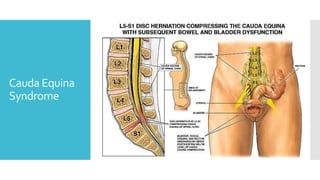
The document discusses a case of a 19-year-old college student who suffered a spinal injury while rock climbing, detailing initial symptoms and emergency response. It provides an overview of spinal cord injuries, including types, mechanisms, and assessment strategies, emphasizing the importance of stabilization and management to prevent further damage. The document also outlines diagnostic imaging and surgical options for treating spinal injuries, stressing the need for immediate and appropriate medical care.