The document provides an overview of cardiovascular assessment including:
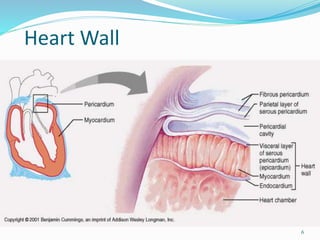
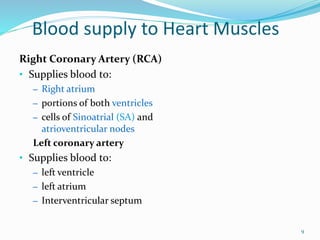
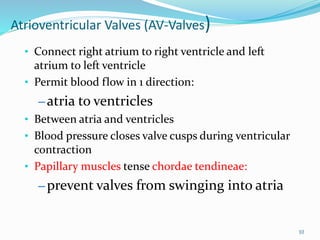
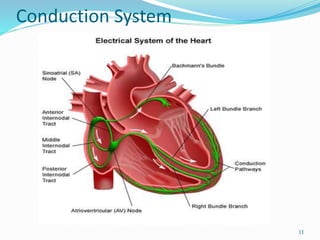
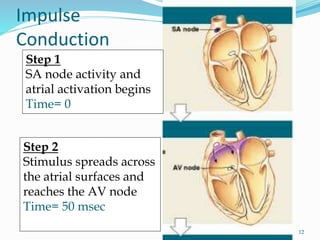
- Reviewing anatomy and physiology of the heart and cardiovascular system.
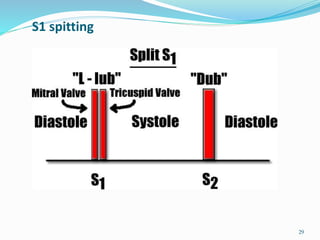
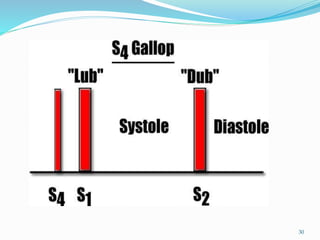
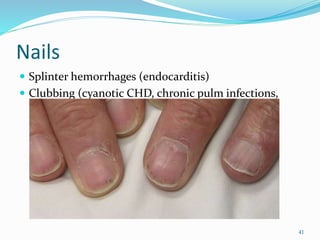
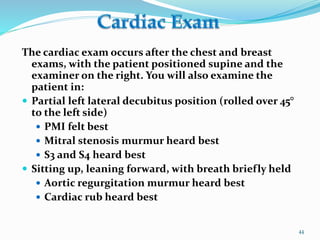
- Demonstrating techniques for cardiovascular examination such as assessing heart sounds, murmurs, and peripheral circulation.
- Analyzing a cardiac patient's health status by taking a thorough history, performing a physical exam, and documenting relevant clinical findings to develop an appropriate care plan.

![ Listen at four basic locations using the diaphragm and bell of
the stethoscope firmly applied to bare skin in a completely
quiet room:
Position:
Sitting, leaning forward, supine & left lateral decubitus
position
Area
Cardiac apex (mitral valve area)
Tricuspid area (left lower sternal border [LLSB])
Pulmonic area (left 2nd ICS)
Aortic area (right 2nd ICS)
48](https://image.slidesharecdn.com/unit3-171221150838/85/cardiac-assessment-48-320.jpg)
![References B ickley.L.S (2011) Bates’ guide to physical examination and history
taking (10th ed).Philadelphia: J.B.Lippincott
Marcus, G. M., J. Cohen, et al. (2007). "The utility of gestures in
patients with chest discomfort." Am J Med 120(1): 83-89.
World Wide Web Page, Martini, F. H. Fluid and Transport [online]
August2, 2008 [cited 2011 January 19]. Available from: URL:
http://library.med.utah.edu/kw/pharm/
53](https://image.slidesharecdn.com/unit3-171221150838/85/cardiac-assessment-53-320.jpg)