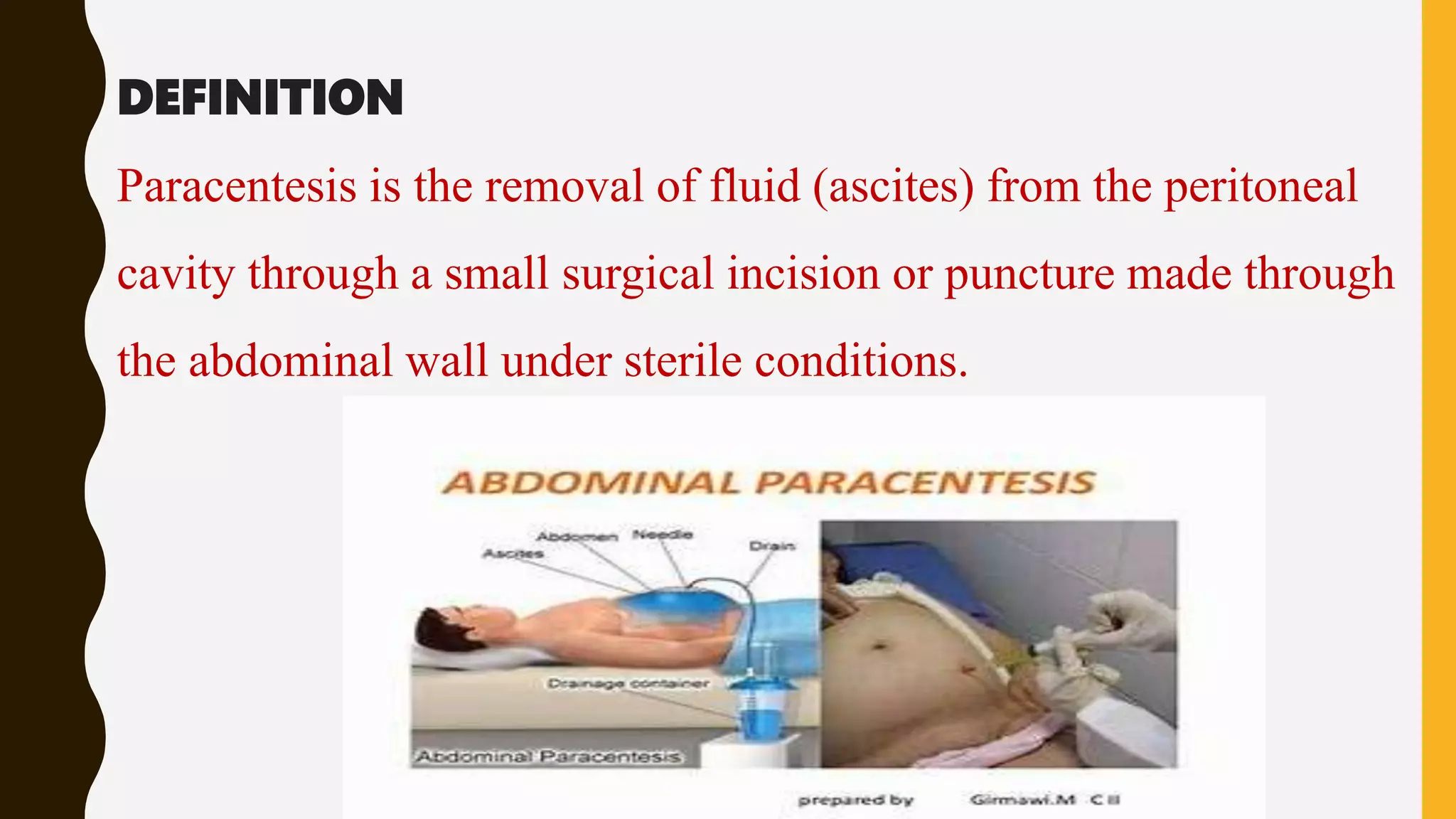
1. Paracentesis is a procedure to remove fluid from the abdominal cavity through a small incision in the abdominal wall. It is performed to relieve pressure from ascites, diagnose the cause of ascites by examining the fluid, and drain fluid in cases of peritonitis.
2. The document outlines the nursing implications for paracentesis including preparing the patient, monitoring them during the procedure, and observing for complications like bleeding or hypotension afterwards.
3. Potential complications of paracentesis include bleeding, infection from organ perforation, low blood pressure from fluid removal, and accidental puncture of blood vessels or organs.