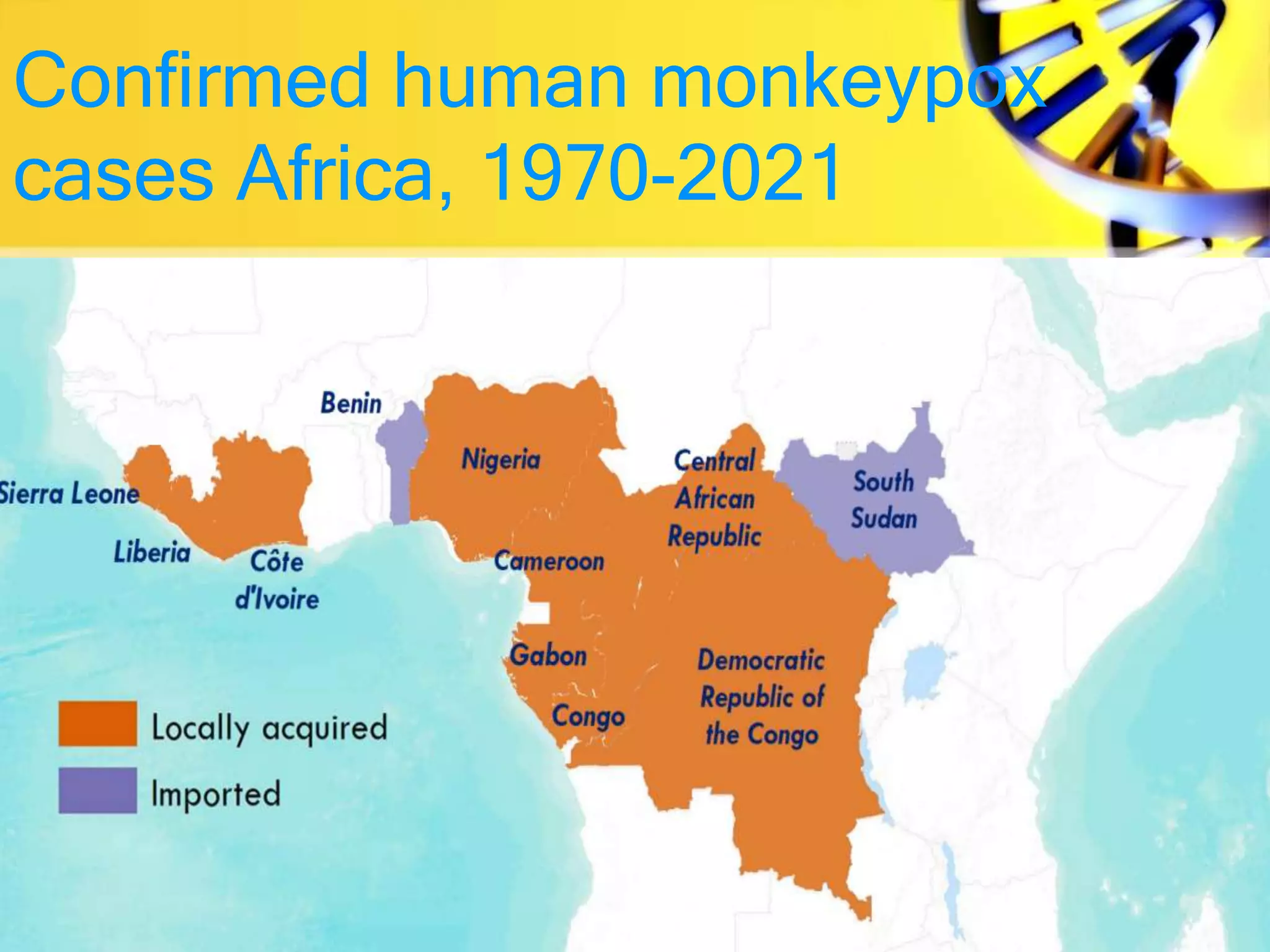
Monkeypox is a viral zoonotic disease primarily found in Central and West Africa, with transmission occurring through close contact with infected individuals, animals, or contaminated materials. Symptoms include fever, rash, and swollen lymph nodes, with the disease typically lasting 2 to 4 weeks and a case fatality ratio around 3-6%. Prevention strategies involve raising awareness and potential vaccination, as the smallpox vaccine has shown effectiveness against monkeypox.