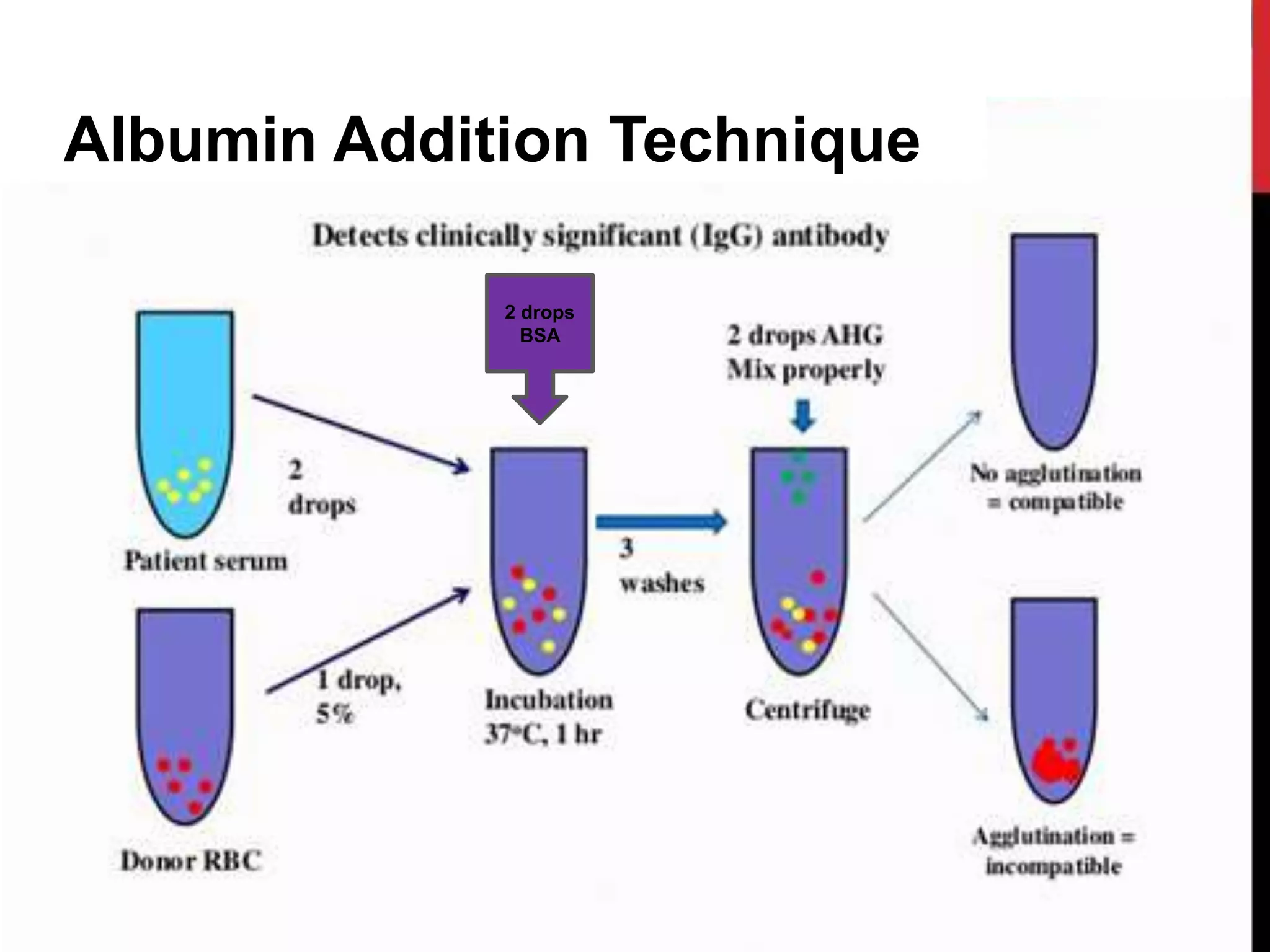
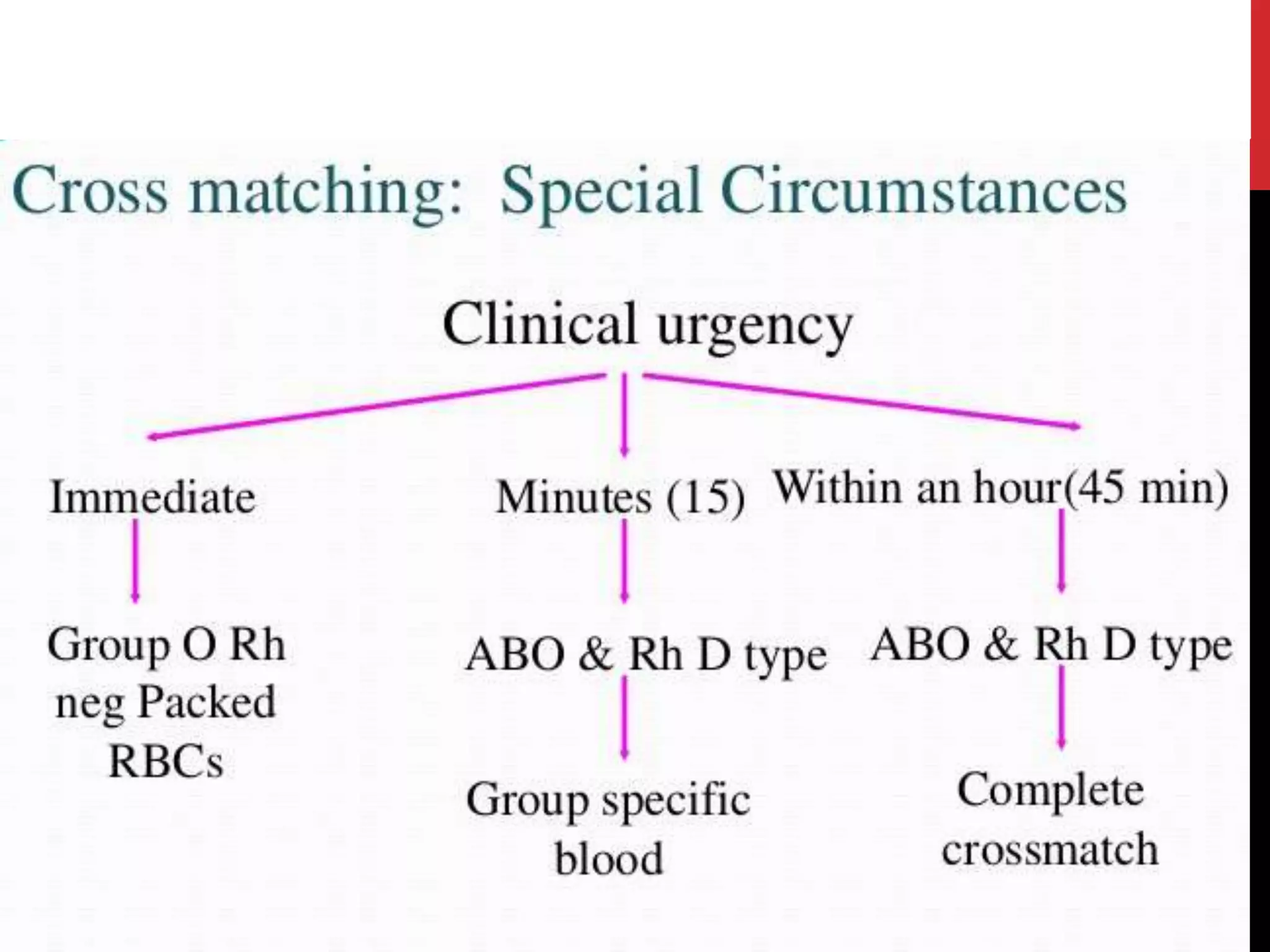
This document discusses cross-matching, which is an important procedure for safe blood transfusion. Cross-matching involves testing a donor's red blood cells with a recipient's serum to check for antigen-antibody reactions. It helps detect atypical or clinically significant antibodies that could cause hemolytic transfusion reactions. There are two main types of cross-matches: major involves donor red cells and recipient serum, while minor uses recipient cells and donor serum. The document outlines different techniques for cross-matching like immediate spin, indirect antiglobulin, and albumin addition, and discusses factors that can cause positive cross-match results.