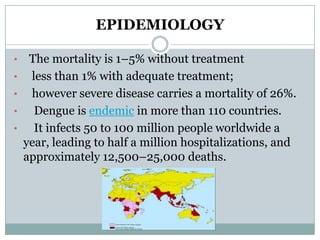
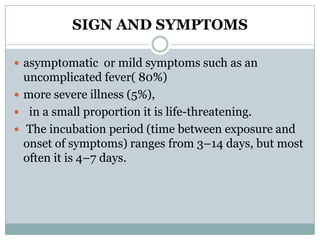
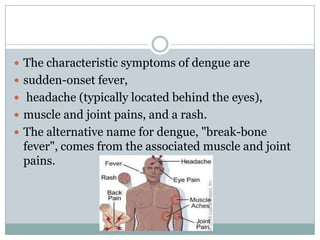
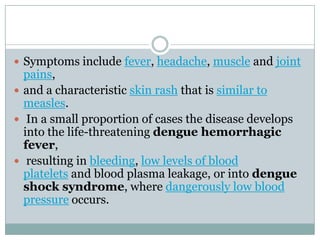
Dengue fever, also known as breakbone fever, is caused by the dengue virus and transmitted by Aedes mosquitoes. It is endemic in over 110 countries, infecting 50-100 million people annually. Symptoms include high fever, headache, muscle and joint pains, and a rash. In a small percentage of cases, it can develop into severe dengue hemorrhagic fever or dengue shock syndrome, which can be life-threatening. There is no vaccine, so prevention depends on controlling mosquito populations and avoiding bites. Nurses play an important role in monitoring patients, providing rehydration and blood transfusions if needed, and educating on prevention.
![ Dengue virus is primarily transmitted
by Aedes mosquitoes, particularly A. aegypti.
These mosquitoes usually live between
the latitudes of 35° North and 35° South below
an elevation of 1,000 metres (3,300 ft).[2] They bite
primarily during the day.
Other Aedes species that transmit the disease
include A. albopictus, A. polynesiensis and A.
scutellaris.
Humans are the primary host of the virus,[2][12] but it
also circulates in nonhumanprimates.[16](https://image.slidesharecdn.com/denguefeverppt-121109034101-phpapp02/85/Dengue-fever-ppt-8-320.jpg)
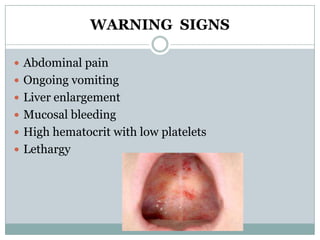
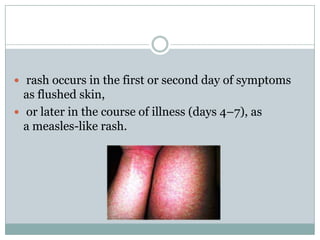
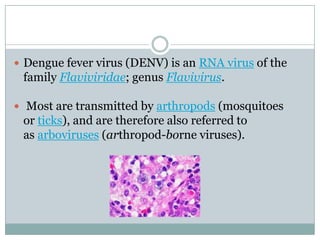
![ Some petechiae (small red spots that do not
disappear when the skin is pressed, which are caused
by broken capillaries) can appear at this point,[9] as
may some mild bleeding from the mucous
membranes of the mouth and nose.](https://image.slidesharecdn.com/denguefeverppt-121109034101-phpapp02/85/Dengue-fever-ppt-20-320.jpg)
![ During this phase there may be significant fluid
accumulation in the chest and abdominal cavity due
to increased capillary permeability and leakage.
This leads to depletion of fluid from the
circulation and decreased blood supply to vital
organs.[9]](https://image.slidesharecdn.com/denguefeverppt-121109034101-phpapp02/85/Dengue-fever-ppt-22-320.jpg)

![DIFFRNTIAL DIAGNOSIS
It can be difficult to distinguish dengue fever
]]
and chikungunya,
a similar viral infection that shares many symptoms
and occurs in similar parts of the world to dengue.
Often, investigations are performed to exclude other
conditions that cause similar symptoms, such
as malaria, leptospirosis, typhoid
fever, and meningococcal disease](https://image.slidesharecdn.com/denguefeverppt-121109034101-phpapp02/85/Dengue-fever-ppt-34-320.jpg)
![ (3) an integrated approach to disease control to
maximize use of resources,
(4) evidence-based decision making to ensure any
interventions are targeted appropriately and
(5) capacity-building to ensure an adequate
response to the local situation.[15]](https://image.slidesharecdn.com/denguefeverppt-121109034101-phpapp02/85/Dengue-fever-ppt-38-320.jpg)