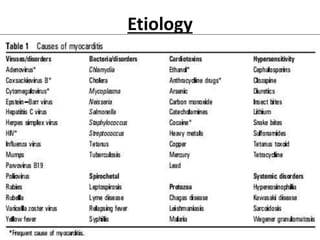
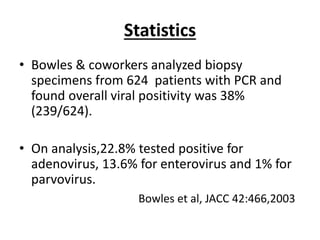
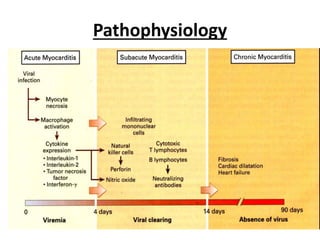
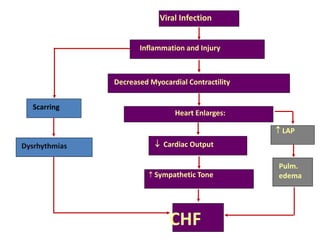
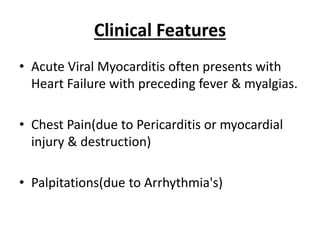
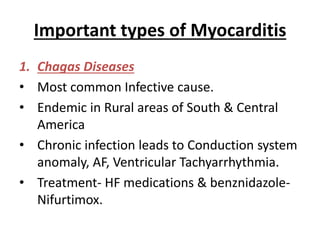
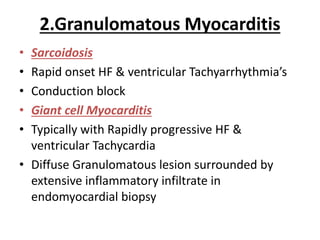
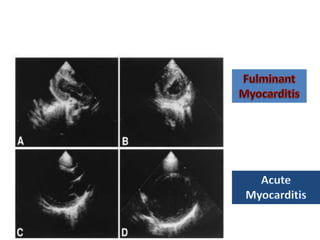
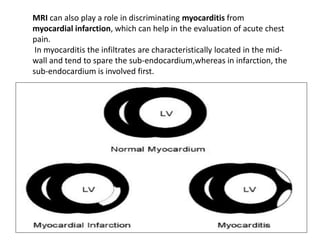
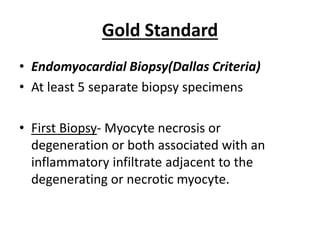
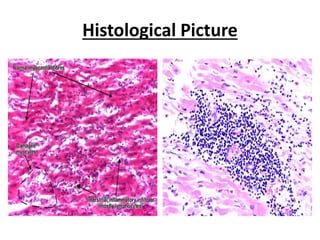
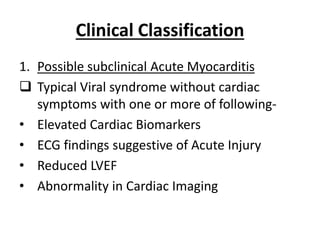
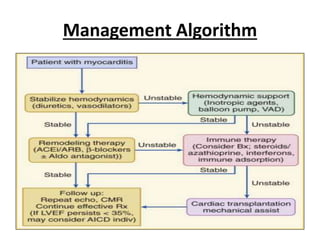
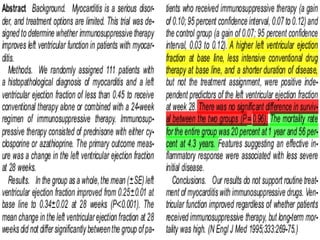
Myocarditis is an inflammatory disease of the heart muscle that is usually caused by viral infections. It can lead to dilated cardiomyopathy and heart failure. Viruses are the most common cause, with adenovirus now more prevalent than coxsackievirus. Myocarditis presents with symptoms of heart failure, chest pain, or arrhythmias. Diagnosis involves EKG, cardiac biomarkers, echocardiogram, cardiac MRI, and endomyocardial biopsy. Treatment focuses on managing arrhythmias and heart failure with medications, while immunosuppression may benefit some forms of myocarditis but not others.