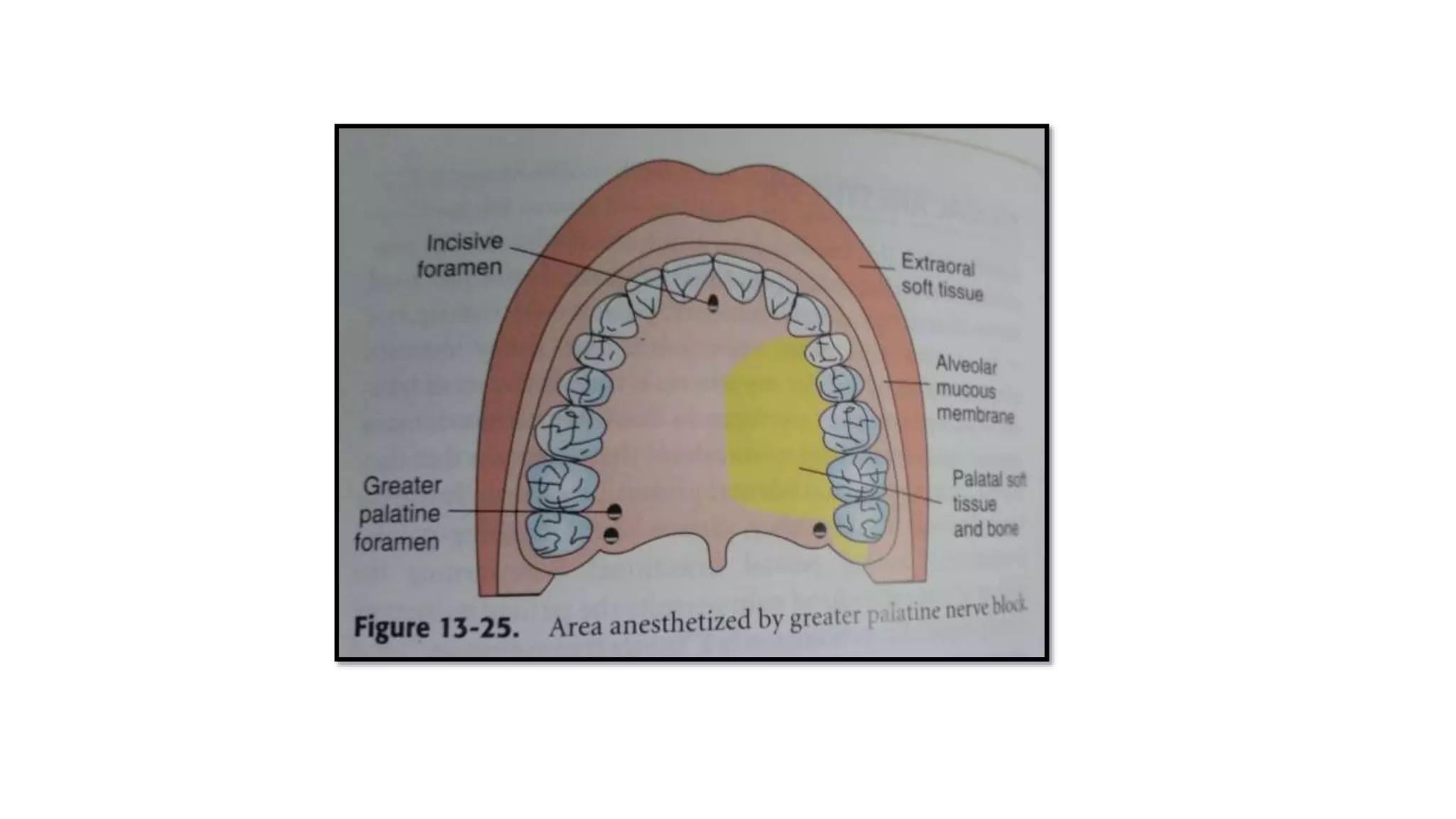
The document provides a comprehensive overview of nerve block techniques specifically focusing on the posterior superior alveolar and greater palatine nerve blocks, detailing anatomical considerations, techniques, indications, contraindications, advantages, and potential complications. The posterior superior alveolar nerve block is primarily used for maxillary molar procedures with a high success rate but may require additional injections for certain roots, while the greater palatine nerve block is utilized for anesthetizing palatal tissues. The document includes procedural guidelines, precautions, and failure correction strategies for both techniques.