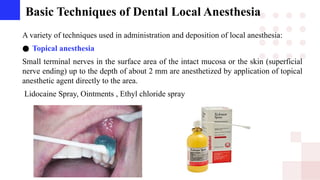
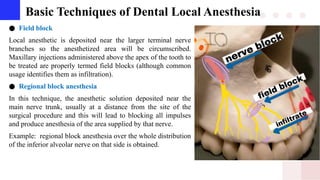
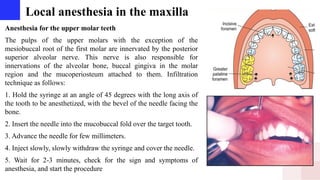
The document discusses the essential techniques and anatomical considerations of dental local anesthesia, highlighting its role in pain management during dental procedures. It covers the major branches of the trigeminal nerve responsible for oral sensation, as well as various local anesthesia techniques, including infiltration, field block, and regional block anesthesia. It provides detailed descriptions of injection techniques for both maxillary and mandibular anesthesia, ensuring effective and safe administration to minimize patient discomfort.



![Maxillary Division (V2)
Branches originating within the pterygopalatine fossa
● The nasopalatine nerve
provide sensation to the palatal mucosa in the region of the
premaxilla.
● The greater palatine nerve
usually located about 1 cm toward the palatal midline, just distal
to the second molar supplying sensory innervation to the palatal
soft tissues and bone as far anterior as the first premolar, where it
communicates with terminal fibers of the nasopalatine nerve.
● The posterior superior alveolar
providing sensory innervation to the mucous membrane of the
sinus, alveoli, periodontal ligaments, and pulpal tissues of the
maxillary third, second, and first molars (with the exception [in
28% of patients] of the mesiobuccal root of the first molar).](https://image.slidesharecdn.com/56197146674322740241-241122054759-5b7e315c/85/basic-techniques-of-dental-local-anesthesia-pptx-4-320.jpg)