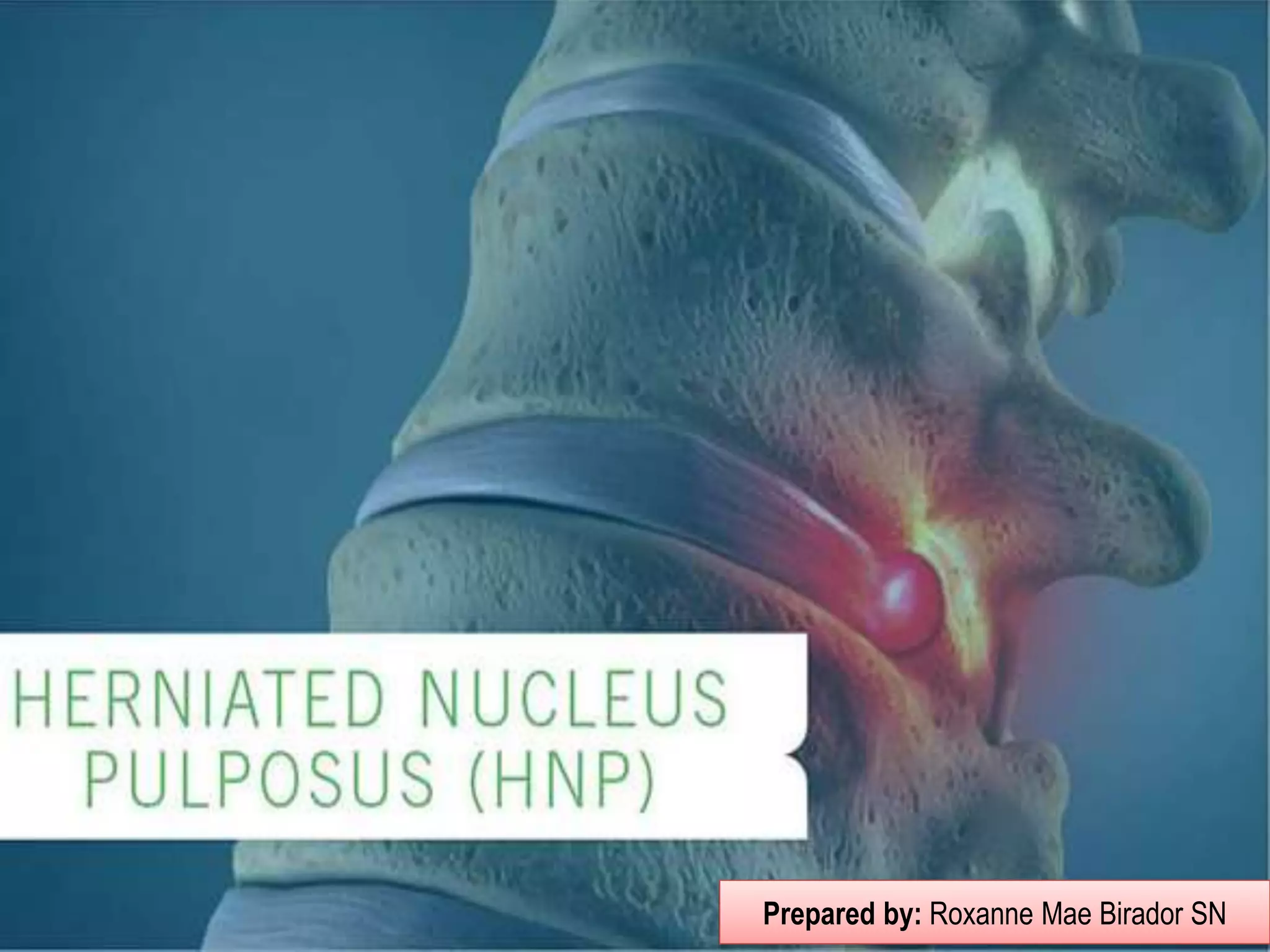
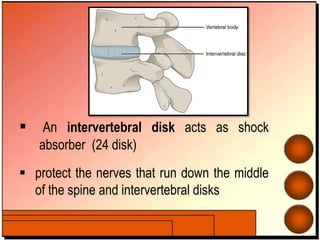
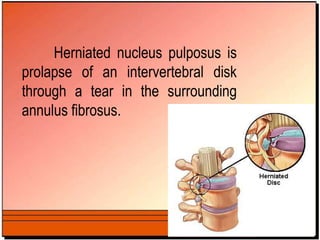
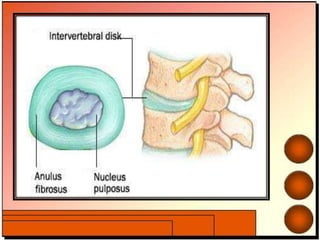
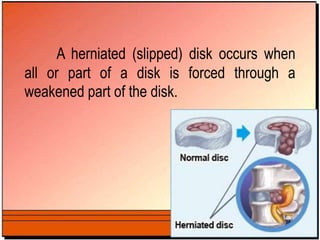
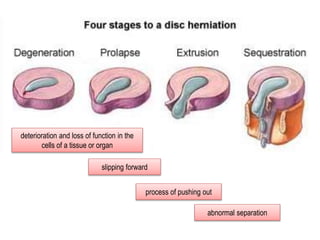
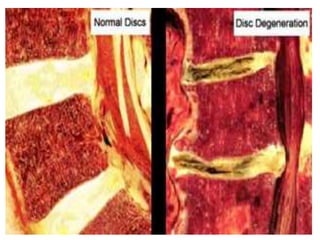
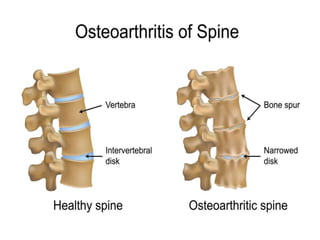
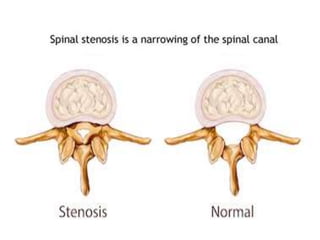
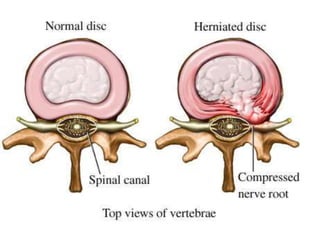
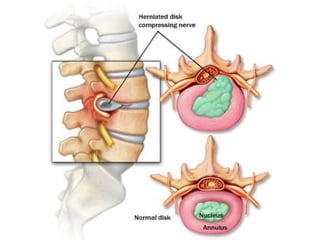
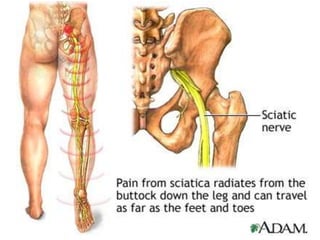
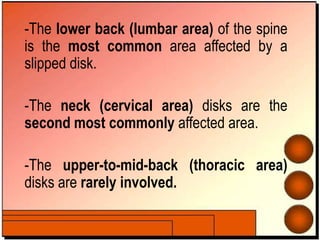
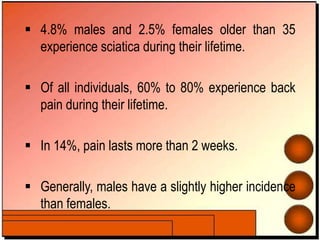
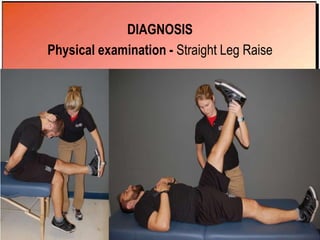
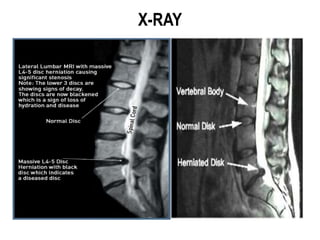
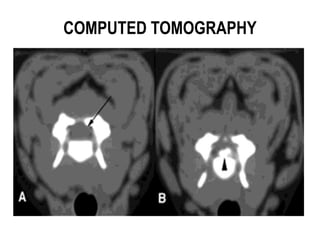
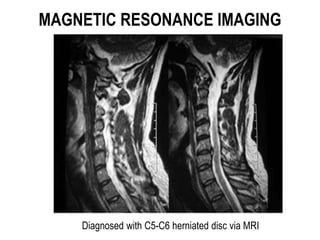
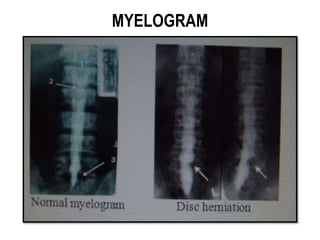
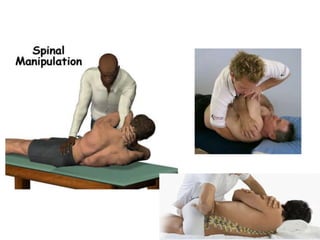
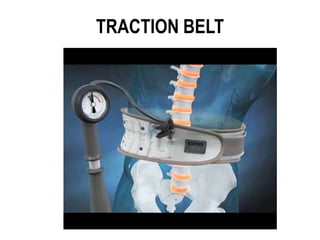
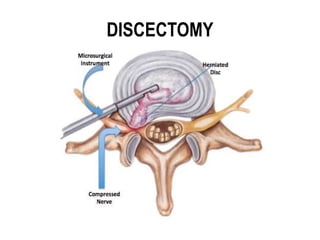
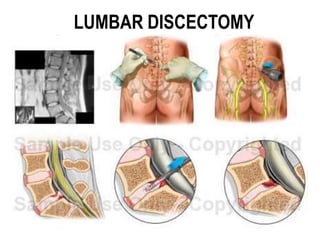
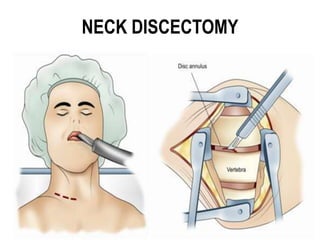
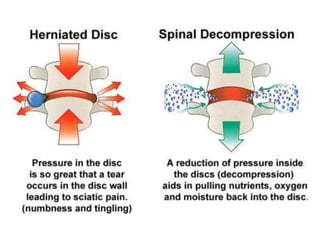
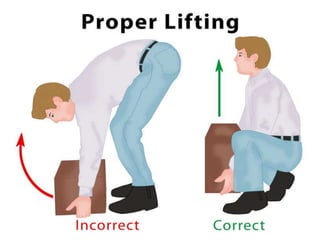
A herniated disk occurs when the inner nucleus pulposus protrudes through damage to the outer annulus fibrosus. Common symptoms include low back pain radiating into the leg. Diagnosis involves physical examination, imaging like MRI, and sometimes electromyography. Treatment options include medications, physical therapy, spinal manipulation, injections, and possibly surgery if conservative options fail. Prevention focuses on education, proper lifting technique, exercise to strengthen the back, and maintaining a healthy weight.