This document provides definitions and information about various types of bacteria important in bacteriology. It discusses obligate aerobes and anaerobes and facultative anaerobes. It also covers specimen collection, gram stain procedure, commonly used agar media, and identification methods like MALDI-TOF mass spectrometry. Key details are provided about important gram positive cocci like Staphylococcus, Streptococcus, Enterococcus, and Streptococcus pneumoniae.

![Streptococcus pyogenes
• Group A beta Streptococcus [GAS]
• Bacitracin KB sensitivity test – inhibited, no growth @ disk
• This test is not specific for Group A , it x-reacts with group C
• PYR (pyrrolidonyl arylmidase) reaction
• Organism spotted onto moist PYR disk
• 2 min – RT incubation
• Add Cinnamaldehyde reagent
• Pink = positive = Strep pyogenes
• This test is not exclusive for Strep pyogenes –
Enterococcus and Staph lugdunensis also (+)
• Therapy : Penicillin or Cephalosporin antibiotics
No resistance reported to these agents
PYR](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-21-320.jpg)
![Strep agalactiae [GBS]
• Pathogen of the elderly – Bacteremia and urinary tract infection
• Pathogen of neonate – in utero or perinatal organism acquisition during
birthing process, infection in @ 1/2000 births
• Early onset – within 7 days
• Late 7 – 28 days from birth process.
• Treatment: Penicillin or Cephalosporin (3rd
generation)
• Pregnant women carry organism in the cervix and/or rectal area (@25%)
• All pregnant must be tested at 35 – 37 weeks of pregnancy.
• Enrichment methods for GBS are standard of practice and must be used
• Swab placed into enrichment broth (LIM) – incubate for 18 hours at 35 ˚C
then subculture onto Blood agar. The broth can also be used as an
enrichment method to for molecular testing methods
• Ampicillin drug of choice for prevention of infection
• Susceptibility testing for alternative therapies
• Clindamycin testing with Inducible resistance testing confirmation](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-26-320.jpg)
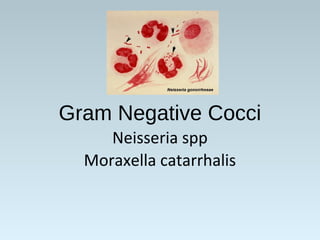
![Neisseria gonorrhoeae
• STD - acute urethritis, endocervix, ocular, rectal,
oropharynx, septic arthritis
• 10 – 20 % female ascend to PID but only 0.5% disseminate
• Gram stain of urethral discharge useful for male diagnosis
• Gram stain of cervix can be problematic due to NF look alike
organisms, primarily Acinetobacter species
• Transport – Appropriate swabs (charcoal) No refrigeration
• Media: Selective Thayer Martin or Martin Lewis agar
• Amplification methods [PCR] increase sensitivity of
detection and superior to culture – standard of practice
• Produces a beta lactamase enzyme and has Chromosomal
resistance mechanisms: Therapy: Ceftriaxone +
Azithromycin or Doxycycline to prevent development of
resistance](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-40-320.jpg)
![•Escherichia coli
• Normal flora in human intestine
• #1 cause of UTI [@80%]
• Bacteremia, neonatal meningitis,
abdominal infections, diarrhea
Biochemicals:
• Spot indole reaction = positive
• Breakdown of Tryptophan found in blood agar
• Green sheen produced on Eosin methylene blue agar
• Pathogen of diarrhea
• Enterotoxigenic E. coli – Traveler’s diarrhea
• Enterohemorrhagic E. coli [0157:H7] - EHEC
• Bloody diarrhea acquired from eating undercooked meat from an
infected cow
• HUS – hemolytic uremic syndrome can result [hemolytic anemia,
thrombocytopenia, and renal failure] particularly in children
• Does not ferment sorbitol – most other E. coli ferment Sorbitol
Green sheen on
EMB agar
Indole positive
Lactose
fermentor](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-53-320.jpg)
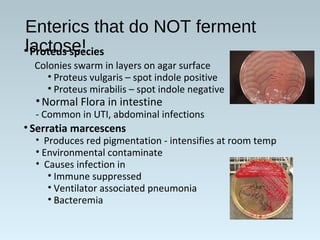
![Glu/lac/suc
fermented
with gas
Glucose
fermented
Glucose
fermented
with H2S
No CHO
fermentation
Non fermenter
Triple Sugar Iron Agar (TSI)– Used to detect
fermentation of glucose, lactose and/or sucrose and
production of hydrogen sulfide [H2S]
Fermentation= yellow medium
Gas = Disruption of the agar
H2S
No fermentation =
Red medium](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-56-320.jpg)
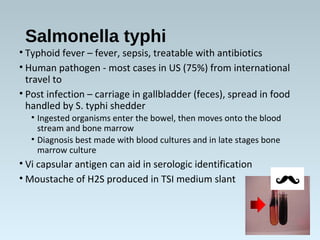
![•Salmonella species
• Diarrhea with +/- fever – polys in the stool
• Infection from eating contaminated food (raw eggs)or
directly from contact with a sick animal
–must ingest large #’s of organisms to make you ill
(1,00,000 bacteria), stomach acid is protective
• Does not ferment lactose
• Produces Hydrogen sulfide on TSI slant and selective agars
• Motile
• Identification based on biochemical reactions and serologic
typing
• Kaufman White serologic typing for speciation of
Salmonella
• O Somatic (cell wall) antigen – Salmonella group “B”
• H flagellar antigens – 2 phases [h1 & h2]
• Vi capsular antigen – Salmonella typhi only](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-57-320.jpg)
![Shigella
• Diarrhea, +/-vomiting, fluid loss, polys and blood in stool
• Infection : Human to human transmission /control with
good hygiene
• Low #’s of organisms make you ill [10 – 100 bacteria]
• Does not ferment lactose
• Non motile
• No H2S produced
• 4 species based on somatic antigen
• S. boydii Group C
• S. dysenteriae Group A
• S. flexneri Group B
• S. sonnei Group D](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-59-320.jpg)
![Salmonella Shigella Agar
(SS agar)
Salmonella and Shigella are
colorless due to lactose not
being fermented – H2S
produced by Salmonella
Hektoen agar –
Salmonella produces H2S [Hydrogen
sulfide] producing black colonies
Shigella – green colonies
Normal flora – orange colored due to
fermentation of lactose (E. coli)
Non-Lactose fermenter
Shigella
Salmonella
Normal Flora
Lactose fermented
H2S](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-60-320.jpg)
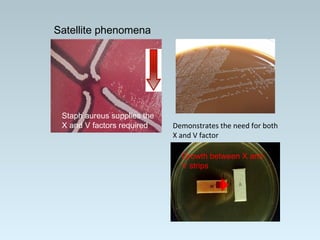
![Haemophilus influenzae
• Transmission – close contact/secretions
• Virulence factor – capsular polysaccharide
• Small pleomorphic Gram negative rod
• Requires 2 nutritional factors for growth:
• X = hemin
• V= NAD (nicotinamide adenine dinucleotide)
• Grows on chocolate agar (has X and V factor)
• Will not grow on 5% sheep’s blood agar
• Requires C0₂ [5 – 8%] for growth
• Effective vaccine targets invasive infections with H. influenzae
type B (HIB) – effectively eliminated most childhood invasive
infections
• Resistance to Ampicillin due to beta lactamase enzyme
productions [25 %], 3rd
generation Cephalosporin becomes the
antibiotic of choice (Cefotaxime or Ceftriaxone)](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-69-320.jpg)

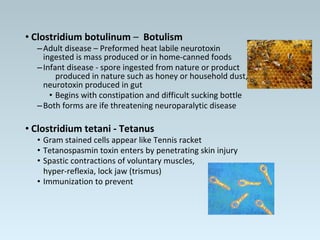
![•C. septicum –
• Bacteremia or Gas Gangrene in patient with underlying
malignancy
• Hematogenous spread from GI tract – no trauma necessary
•C. difficile –
• Disease: antibiotic associated colitis, pseudomembranous
colitis from toxin production
• Toxin A – enterotoxin causing fluid accumulation
• Toxin B – potent cell cytotoxin – primary virulence
• Binary toxin – so called Nap1 strain is produces
larger amount of toxin
• Diagnosis of infection:
• EIA methods [toxin A/B] are insensitive but detect active toxin
• PCR methods [toxin A/B] are more sensitive, detect toxin genes
• Culture – Cycloserine, Cefoxitin, Fructose Agar [CCFA]
• Infants have @ 70% colonization rate – do not test](https://image.slidesharecdn.com/webpagebacteriology2018update-180410014430/85/Bacteriology-2018-Update-97-320.jpg)