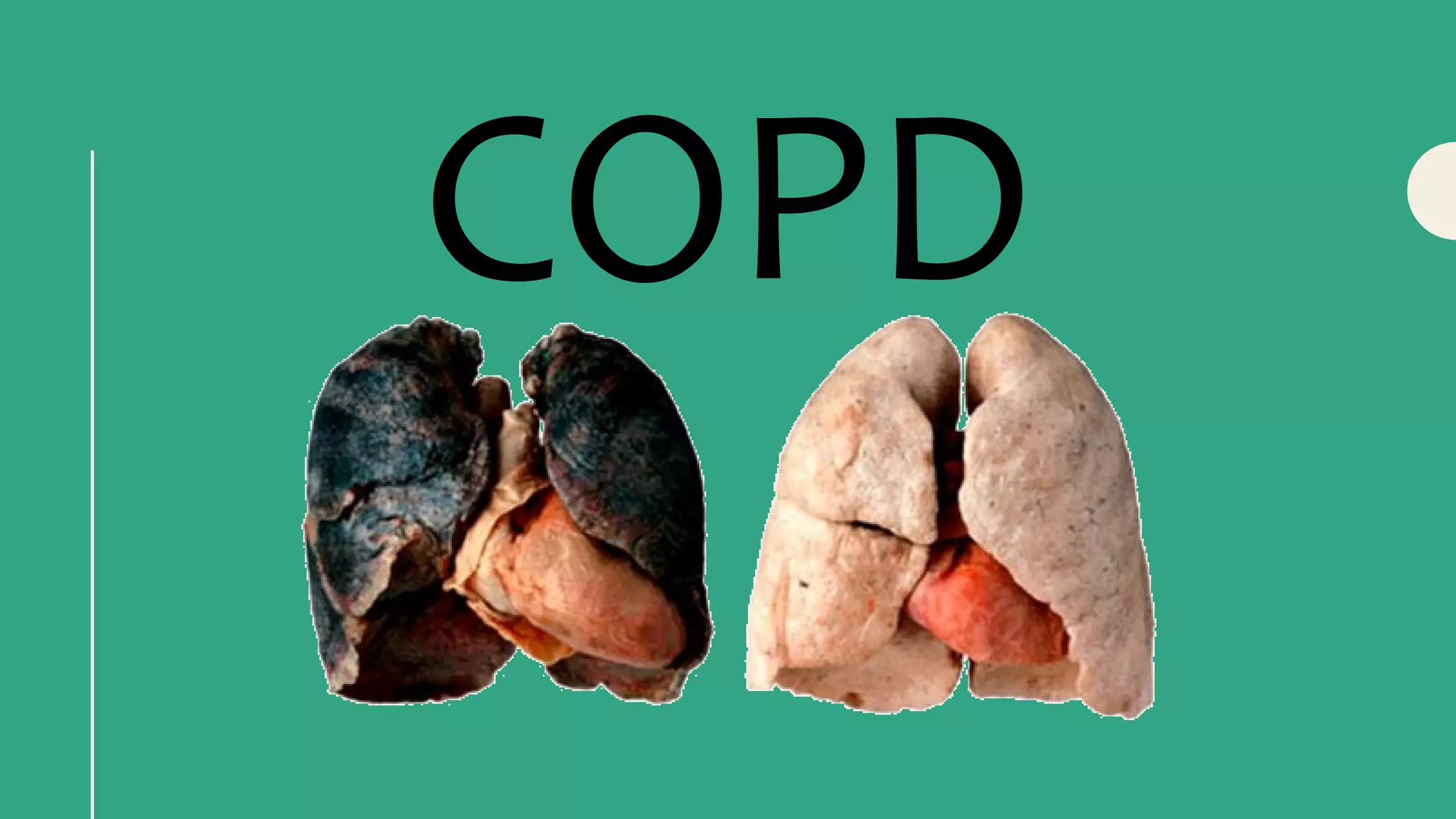
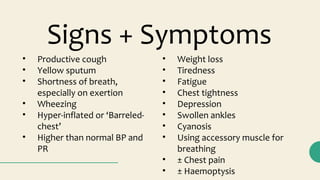
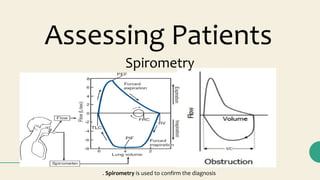
COPD is a lung disease characterized by chronic bronchitis and emphysema that causes obstruction of airflow in the lungs. The main symptoms include productive cough, wheezing, shortness of breath, and fatigue. Smoking is the primary risk factor. Diagnosis involves taking a medical history focused on smoking status and performing spirometry to confirm airflow limitation. Management consists of smoking cessation, bronchodilators, steroids, vaccinations, and following up on inhaler techniques and for exacerbations.