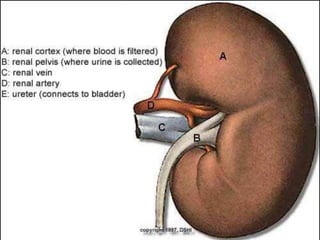
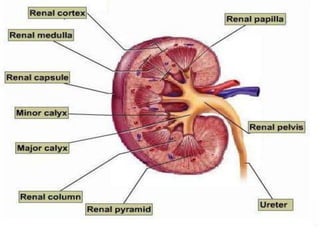
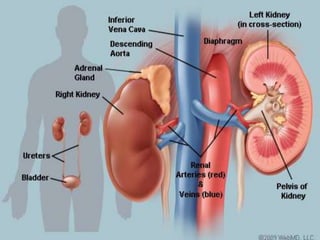
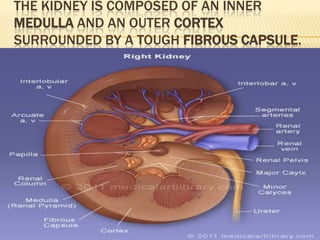
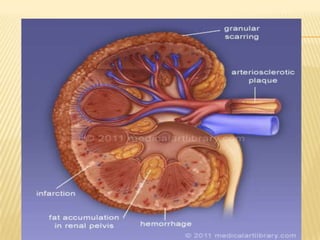
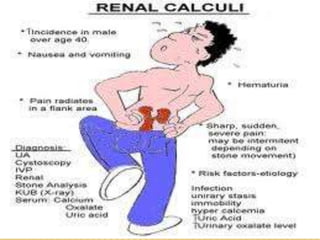
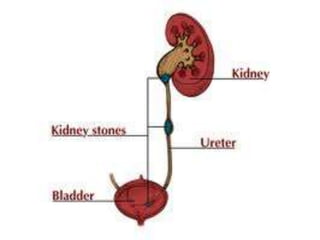
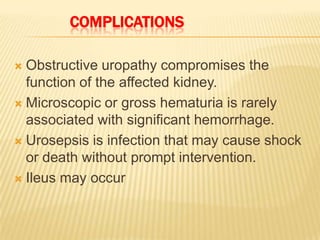
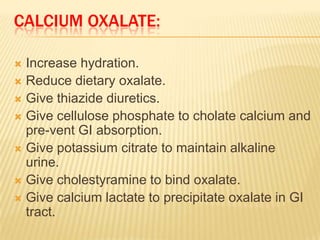
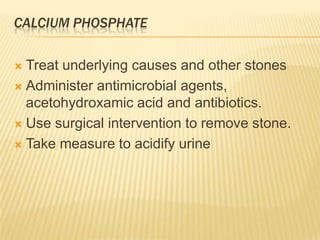
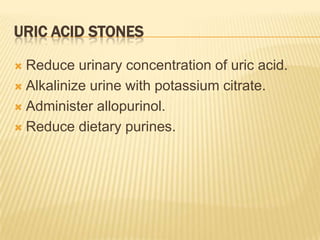
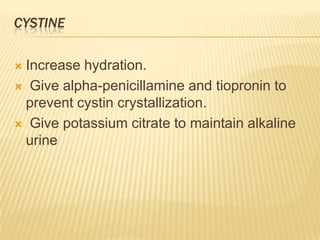
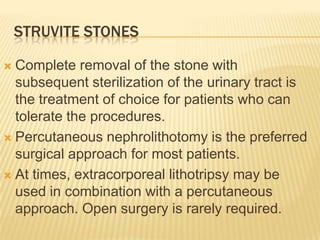
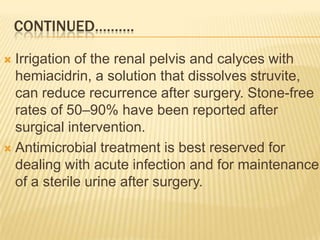
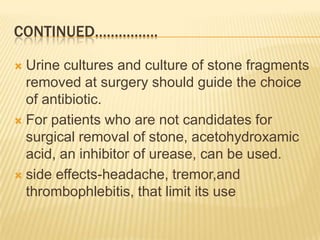
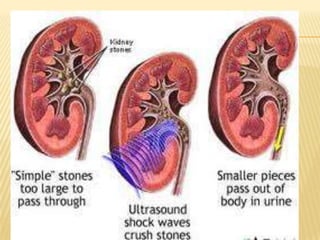
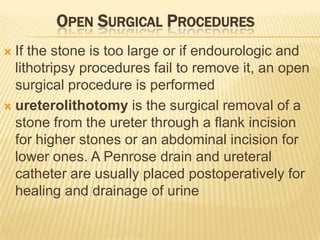
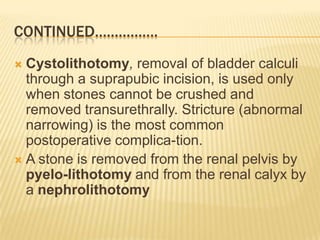
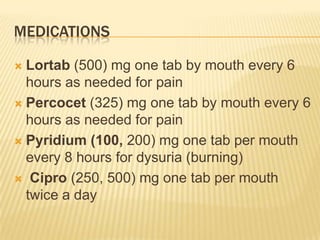
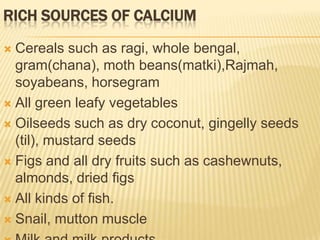
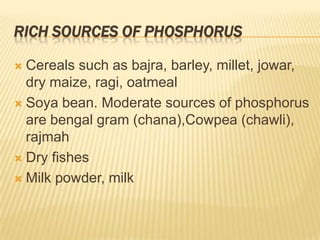
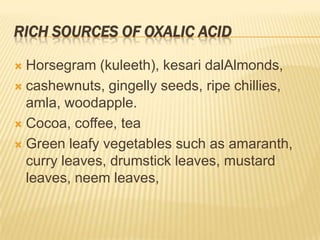
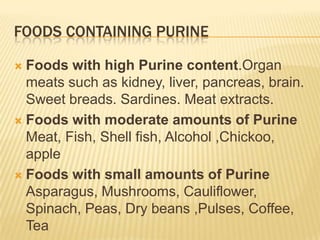
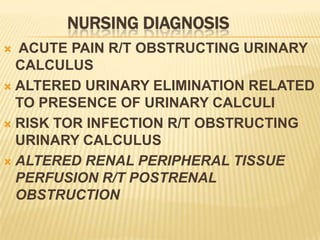
The document describes the anatomy and physiology of the urinary tract and kidney, risk factors and types of kidney stones, and methods for diagnosing and treating stones, including increasing fluid intake, altering diet, using medications to change urine composition, and surgically removing stones with procedures like ureteroscopy and lithotripsy. Kidney stones form when substances like calcium, oxalate, and uric acid become supersaturated in the urine and crystallize into solid masses.